Showing posts from category maternal health.
-
IPPF and Partners Connect Reproductive Rights With the Environment and Development
›A new framework for sexual and reproductive health is needed, argued panelists in a recent event at the Wilson Center, and the Rio+20 conference on sustainable development would have been the place to start. An international consensus around women’s human rights was developed at the International Conference on Population and Development in Cairo in 1994, but Carmen Barroso, director of the International Planned Parenthood Federation’s Western Hemisphere Region, said there has been slow implementation, little funding, and furthermore the world has changed significantly since then.
Barroso was joined by Latanya Mapp Frett, vice president of Planned Parenthood Global, as well as two representatives of Planned Parenthood partner organizations, Marco Cerezo of FUNDAECO and Ben Haggai of Carolina for Kibera.
New challenges to the reproduce rights landscape include the rapid spread of HIV/AIDS and decreased funding for international programs. But new opportunities include rapid dissemination provided by the internet and globalization and a subsequent mobilization of youth. “Young people are the largest cohort in history,” Barroso said in an interview with ECSP, both in absolute numbers and in percent of the population. “We have a historical opportunity [to incorporate] them in these decision-making processes.” Additionally, gender and health issues are incresaingly seen by many as linked with the environment and development.
Intersection of Health and the Environment
Marco Cerezo’s FUNDAECO (Foundation for Ecodevelopment and Conservation) is an example of Planned Parenthood’s partnership with other organizations. Based, in rural Guatemala, they shifted from primarily focusing on conservation and sustainable development to incorporating women’s health after finding a vicious cycle of poverty, high fertility, and environmental degradation in the places they worked.
Women’s health was so dire it was holding development back, Cerezo said. “Sustainable community development will not be possible without the education, empowerment, and support to rural women,” they write in their mission statement.
FUNDAECO now acts as a model for the intersection between reproductive health and the environment. Cerezo reported that once women are healthy and empowered through clinics established by FUNDAECO, they become more active in all aspects of the community, including ecological preservation.
Building Healthy Communities
Ben Haggai, who works in Nairobi’s biggest slum, Kibera, further reiterated the need for integrated programs. Carolina for Kibera has a number of programs to improve the quality of life for residents, he said, and has a particular focus on youth with sports associations and education programs.
Youth are the best reproductive health educators, Haggai said, as they are able to talk frankly with their peers. The NGO trains peer youth educators to reach out to community members about reproductive health and other issues like substance abuse. Since the young people work as volunteers, Haggai said, they are motivated only by a desire to improve their communities.
A Natural Intersection
Latanya Mapp Frett agreed that sexual and reproductive health aligns quite naturally with issues of sustainability. “We try to work in the countries overseas in Latin America and Africa where we focus particularly on non-traditional health sectors,” she said in an interview with ECSP following the panel. “One of those sectors is the environment.”
While emphasizing that contraceptive use is a cost-effective way to ensure sustainable development, Mapp Frett cautioned against framing sexual and reproductive health only in the context of reducing fertility. While this may have been common in the past, she noted, it’s important to ensure that women have the right to make childbearing choices for themselves.
Mapp Frett also urged policymakers in the United States to look to developing countries for intersections between development, the environment, and reproductive health. She said that Planned Parenthood’s partner organizations, including FUNDAECO and Carolina for Kibera, have found these connections and successfully partnered with already existing networks like churches to more effectively reach the community.
Translating Into Effective Action
Each member of the panel spoke about the challenge of articulating the need for sexual and reproductive health programs to people outside the field. Barroso mentioned research conducted by Brian O’Neill which found that meeting the current unmet need for contraception would slow population growth enough to reduce emissions by 17 percent.
Cerezo emphasized the importance of consensus among the staff of a given organization, saying it is difficult to make a case to agronomists and farmers if a culture clash exists within the institution. Haggai agreed, adding that focusing on reproductive issues is an important measure of prevention which helps protect both the environment and the health of women in a community.
For Mapp Frett, women’s reproductive and sexual health is indivisible from other aspects of development. “As you talk about sustainable development, you talk about ensuring that women are empowered to make sure that our earth is sustainable,” she said.
Assessing Rio+20
The panel took place before the UN Conference on Sustainable Development got underway in Rio. Participants had high hopes for a renewed focus on gender and reproductive rights at the conference. Unfortunately, language on reproductive rights was first weakened and then omitted entirely from the final outcome document (see the account written by ECSP’s Sandeep Bathala at Rio for more on the conference).
While pressure from the Vatican and the G-77 kept reproductive health out of the outcome document, it was not entirely forgotten at the conference. A number of side events highlighted the importance of reproductive rights, especially in the context of the environment and development.
Hillary Clinton also re-affirmed U.S. commitment to access to contraception and reproductive health care. “Women must be empowered to make decisions about whether and when to have children,” she said at the conference on Friday. “And the United States will continue to work to ensure that those rights are respected in international agreements.”
Clinton shared the urgency expressed by the panelists at the Wilson Center. “There is just too much at stake, too much still to be done,” she said. “We simply cannot afford to fail.”
Event Resources:Sources: FUNDAECO, UN Conference on Sustainable Development, U.S. Department of State.
Photo Credit: Sean Peoples/Wilson Center. -
Pop at Rio+20: Text Finalized, Population-Sustainable Development Links Left Out?
›June 21, 2012 // By Sandeep BathalaWhile I was visiting with youth peer educators yesterday with the Brazilian Society for Family Welfare in the Cachoeirinha favela (see Vicky Markam’s post for details – we were on the same trip), UN member states reached consensus in the Rio+20 negotiations. But, according to reports, although the outcome document includes some mention of reproductive health, gender equality, and women’s empowerment, it fails to explicitly recognize the link between reproductive rights and sustainable development.
Many women’s rights and health observers have, from the start, encouraged this link.
Karen Newman, speaking to ECSP in April during the Planet Under Pressure conference – a precursor to Rio – said she hoped this week would offer an opportunity to look at “sustainable development in the round” and “re-identify family planning as a core development priority,” given its human rights and health implications and relationship to population growth.
Jenny Shipley (Former Prime Minister of New Zealand) wrote just yesterday on CNN that “we are at a moment in history where we still have time to make a difference. It is essential that the global discussion in Rio not be blind to the potential solutions that access to voluntary family planning could offer to many of the world’s problems.”
“We can no longer afford this outrageous oversight, driven by old-fashioned tradition, discrimination, and pure ignorance,” said Gro Harlem Brundtland (Former Prime Minister of Norway and Former Head of the World Health Organization) at a side event on Monday. “Now is the time to agree to unleash the largest untapped potential for sustainable development and stop all discrimination against women and girls.”
But now that preliminary agreement on the outcome text has been reached, reports have filed in that the connection many were hoping for is absent. Zonibel Woods, blogging on RH Reality Check, wrote:From the start of the negotiations, gender equality and women’s human rights, including reproductive rights, have continuously been challenged by a few governments, claiming that [these] had “nothing to do with sustainable development.”
The lack of consensus among the wider international community may also undercut efforts to highlight reproductive rights in the post-2015 Millennium Development Goals/Sustainable Development Goals framework and as governments ready for the follow-on to the International Conference on Population and Development in 2014. A concrete link to “sustainable development,” whatever form that takes, would help ensure that reproductive health is not side-lined.
This debate continued until the last few hours of the negotiations. In the end, the text includes a re-affirmation of both the Cairo and Beijing agreements, but it falls short by failing to recognize that reproductive rights are also critical to the achievement of sustainable development. If a woman cannot decide if and when to have children and if she is not provided with the reproductive health care that is her human right, it is challenging to contribute to sustainable solutions for the planet.
Immediately following the adoption of the text, women gathered and protested at Rio Centro, the main venue for the conference, and advocacy continues.
Heads of state will in all likelihood sign on to the outcome document by tomorrow (it could technically still be changed, but that appears unlikely). I will keep you posted on the final outcome and will be taking notes at a side-event this afternoon by USAID, the Aspen Institute, and Center for Environment and Population on the demographic dividend and sustainable development, which promises to be spirited given today’s news. You can tune in live to the webcast of that event at 2:30 EST on Ustream.
Sources: AllAfrica, Aspen Institute, CNN, IRIN, RH Reality Check, U.S. Department of State, USAID.
Photo Credit: United Nations Photo. -
Africa on the Move: The Role of Political Will and Commitment in Improving Access to Family Planning
›Excerpted below is the adapted abstract, by lead authors Eliya Msiyaphazi Zulu and Violet Murunga. The full report is available for download from the Wilson Center’s Africa Program.
Despite commitments to the program of action for the 1994 International Conference on Population and Development and Millennium Development Goal 5 (focused on maternal and reproductive health), little progress has been made in improving access to family planning and slowing rapid population growth in Africa. Lack of political will has been highlighted among the key factors behind the lackluster performance in addressing these sensitive development issues. However, the situation is changing with some African governments embracing family planning as a key tool for improving child and maternal health, slowing population growth, preserving the environment, and enhancing broader efforts to alleviate poverty.
This study examines factors that have propelled the change in attitudes of some political leaders to champion family planning, assesses how such political will has manifested in different contexts, and explores how political will affects the policy and program environment. Mixed policy analysis methods were employed, including desk review of policy and program documents and stakeholder interviews conducted in Ethiopia, Malawi, and Rwanda – three countries that have made phenomenal progress in increasing contraceptive use in the recent past.
Lessons from this study will help galvanize efforts to improve access to reproductive health services in countries where little progress is being made. The results provide useful insights on the dawn of a new Africa where strategic political leadership is playing an increasingly valuable role in overcoming the continent’s longstanding development shackles. The study shows that political will is mainly changing due to increased availability of evidence showing that high population growth undermines efforts to alleviate poverty and hunger as well as investments in the quality human capital that least development countries desperately need in order to transform their economies.
The high sensitivity about childbearing and suspicions regarding the intentions of western development partners in promoting family planning in order to slow population growth are dissipating as more Africans are opting to have fewer children and demanding family planning. This study points to the need for global development partners to be much more cognizant of the drivers of Africa’s emerging success and focus their development assistance on enhancing, nurturing, and highlighting local leadership traits, capacities, and systems that are producing positive results, as well as support governments that have embraced family planning to ensure that no woman has an unwanted pregnancy due to lack of family planning.
Download the full report from the Wilson Center. -
Family Planning and Results-Based Financing Initiatives
›“Family planning means healthier moms and kids – and it’s good for development too,” said Lindsay Morgan, a senior health analyst at Broad Branch Associates, a healthcare advocacy group. But any number of hurdles can keep women from accessing family planning services. Morgan spoke at a May 21 discussion about results-based financing (RBF) programs, which aim to address hurdles on both the supply and demand sides of the equation in developing countries by incentivizing the provision of a variety of quality services while removing barriers to access for women in need of those services.
Removing Barriers to Providing and Using Family Planning Services
Incentives in RBF programs can come in a variety of forms – like subsidies or fees paid to clinics or vouchers sold to women, said Morgan. In Burundi, for example, under a pilot program rolled out across three provinces in 2006, health facilities receive payments for each patient that uses a modern method of contraception. In 2009, the government and international partners began scaling up the program to a nationwide level. In addition to expanding the program’s geographic reach, the scale-up incorporated new payment criteria to better incentivize quality of care (as opposed to just quantity) and longer-lasting methods of contraception.
Since the RBF pilot began, maternal and child health indicators have improved. The number of children being fully immunized is up, as is contraceptive prevalence, said Morgan. Additionally, those immediate results can lead to a slew of additional benefits down the line. For instance, improving modern contraceptive prevalence is one of the most cost-effective interventions available for reducing maternal death, she said.
In nearby Kenya, the health ministry leads a voucher system across four districts and two Nairobi slums to help some of the country’s poorest women afford maternal healthcare, family planning, and gender-based violence services.
The program is “written into large policy documents [and] strategic pieces,” including Vision 2030, a long-term government-wide strategy document “unveiled in 2008 as a way to reach middle-income country status by 2030,” said Ben Bellows, a reproductive health associate at Population Council Kenya. The government’s emphasis on the voucher program as more than just a health initiative is an acknowledgment of the downstream impact that improved maternal and reproductive health can have on the country’s development, he said.
“An Equity Gap in Family Planning”
However, the fact that the voucher program is needed at all is evidence of “an equity gap in family planning,” Bellows said. Access to family planning services can be significantly skewed depending on a woman’s income level, he said, pointing to a recent article in The Lancet assessing health inequalities in 12 different maternal and child health services across 54 priority Millennium Development Goal countries.
The equity gap reflects “an interesting problem with development,” said Bellows: Though low-income countries are converging with higher income countries, in terms of economic growth rates and income levels “the benefits of growth aren’t being evenly distributed.” The Africa Progress Panel’s annual report, released last month, echoes that point, he said.
“Governments are failing to convert the rising tide of wealth into opportunities for their most marginalized citizens,” the report concludes, and “unequal access to health, education, water and sanitation is reinforcing wider inequalities.”
Kenya’s voucher system is designed to help shrink that gap. Among the poorest of the poor – those benefitting from the system – inequalities are dropping, even if on a broader scale, inequity still exists between poor and wealthy Kenyans. “We’re seeing lower inequalities of service in areas exposed to the voucher,” said Bellows.
“RBF supports progress on a path towards universal health coverage,” said Beverly Johnston, the senior policy advisor at USAID’s Office of Population and Reproductive Health. And within the context of family planning “the whole idea is to level the playing field” so that all contraceptive methods are equally readily available to the women seeking them.
“A Catalyst for Change” in Family Planning
In addition to addressing equal access concerns, RBF programs can serve as “a catalyst for change…to stimulate quality of care and quality of family planning counseling in particular,” said Johnston.
A commonly cited hurdle to better family planning access is social norms that support large family sizes or otherwise limit a woman’s ability to space or limit her pregnancies. Given community health workers’ unique roles within their communities – “often on the front lines…where many of these social taboos and barriers exist,” as Morgan described – simply strengthening their training, and in turn improving the quality of care that women receive, can help counter norms that might otherwise prohibit access to family planning.
As more women receive higher quality care, norms dissipate even further, said Morgan. “There is evidence that [quality of care] is strongly associated with a woman’s decision to choose a method to use, to continue to use it, and to recommend it to others.”
“Rights Are Tantamount”
One trap RBF programs need to be aware of is over-incentivizing expansion of coverage to the detriment of quality or individual women’s concerns about what makes sense for them, said Johnston.
“Rights are tantamount,” she said. In order to ensure that rights are upheld, programs must reflect and be sensitive to local histories and local needs – particularly given the fact that some countries have had “a history of coercive programs and policies.”
Ultimately, “we really look at RBF as just one tool,” said Johnston. “RBF is not for every place and every context,” and neither is family planning’s place in RBF programming.
As one tool of many, RBF programs are gaining prominence as a way to meet MDGs related to maternal and child health. Bellows sees RBF’s importance lasting long past that 2015 deadline, though.
“The high inequity that we witness across many low-income countries, and the ability of targeted mechanisms [like Kenya’s voucher program] to address that, suggest that this may be a kind of generalized solution,” he said. “Obviously it will be context specific in the way in which it is rolled out, but the strategy of incentivizing clients and providers suggests that there’s some sort of globalized solution that could be considered for this widespread challenge.”
Event Resources
Photo Credit: Sean Peoples/Wilson Center. -
Carl Haub, Behind the Numbers
Republic of Congo Demographic and Health Survey Shows High Maternal Health, But No Fertility Decline
›June 5, 2012 // By Wilson Center StaffThe original version of this article, by Carl Haub, appeared on the Population Reference Bureau’s Behind the Numbers blog.
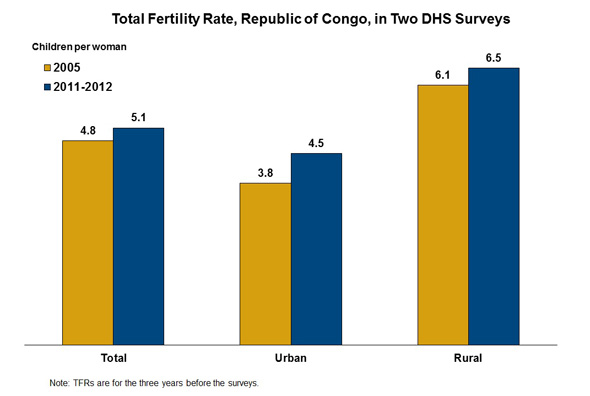
The Congo (Brazzaville) 2011-2012 Demographic and Health Survey (DHS) is the second DHS taken in the country and the preliminary report has just been released. The survey interviewed 10,819 women ages 15-49 and 5,145 men ages 15-59 from September 2011 to February 2012. A major finding of the survey was that fertility has not declined in the country since the previous DHS in 2005. The total fertility rate (TFR) report in the recent DHS for the three year period before the survey was 5.1 children per woman, 4.5 in urban areas, and 6.5 in rural areas. This appears to represent an increase in the TFR since 2005 but the survey report cautions that there is likely to have been some understatement of the actual level of childbearing in the 2005 survey, particularly among women ages 25-29.
Rural women accounted for two-thirds of those interviewed in the most recent survey. The rather high TFR is reflected in the desire for large families. Among women with five living children, only 37.3 percent said they did not wish to have additional children. An additional 9.8 percent of that group said they were incapable of conceiving, however.
In the survey, 44.7 percent of currently married or in-union women said that they were using some form of family planning and 20 percent were using a modern method. The most common type of modern method was the male condom at 12.3 percent, a rather unusual pattern of contraceptive use in Africa. That was followed by the pill at 2.9 percent and injectables at 2.8 percent. This continues the often-observed preference in sub-Saharan Africa for methods to space births, not necessarily to limit them. The use of modern contraception was 24.6 percent in urban areas and 11.7 percent in rural areas. Modern contraception rose since the 2005 DHS when it was reported at 12.7 percent and the condom was also the most frequently used method at that time. The prevalence of HIV was reported in the 2009 AIDS Indicator Survey at 4.1 percent for women ages 15-49 and 2.1 percent of men of the same age group.
Continue reading on Behind the Numbers.
Sources: MEASURE DHS.
Image Credit: Carl Haub/Population Reference Bureau. -
USAID’s New Global Health Framework and Delivering Equity in Health Interventions
›USAID’s new Global Health Strategic Framework, Better Health for Development, lays out the agency’s major health priorities for the next five years. “Core global health priorities” include reducing maternal mortality, ensuring child survival and nutrition, fostering an “AIDS free generation,” and fighting infectious diseases. Family planning and reproductive health is listed as a key area for bilateral engagement. In particular, the strategy hopes to continue to “graduate” countries from the agency’s family planning program, which since the 1980s has transitioned 21 countries into local ownership of family planning support. The strategy also takes stock of the shifting global health environment, noting the rise of the “BRICS” countries as new donors and the need to strengthen public health systems in developing countries. “Already, private payments account for 50-80 percent of total health spending in Africa and Asia, leading to system inefficiencies, inequitable access, and health costs that prove catastrophic to individuals and families,” the report reads. In order to achieve its priorities within this context, the document sets out a number of strategies, including a focus on program sustainability, the empowerment of women, and integrated approaches to development. Health, it says, “cannot be isolated from other development challenges.”
Speaking of health interventions, a team of researchers led by Aluisio Barros of the Federal University of Pelotas, Brazil, recently compared coverage data from more than 50 countries against an index of household wealth to estimate the most and least equitable interventions. The study, “Equity in Maternal, Newborn, and Child Health Interventions in Countdown to 2015: A Retrospective Review of Survey Data From 54 Countries,” published in The Lancet, found that “interventions with similar levels of overall coverage often have very different degrees of inequality.” According to the data, “the most inequitable indicator was skilled birth attendant, followed by four or more antenatal care visits, whereas the most equitable was early initiation of breastfeeding.” For example, though the average for attendance by a skilled birth attendant was 53.6 percent across the entire sample, the wealthiest fifth had an 84.4 percent coverage rate and the poorest stood at 32.3 percent. “Interventions that are usually delivered in fixed health facilities…tend to be the most inequitably distributed,” write the authors, with geographical access, financial barriers, and discrimination appearing as likely obstacles for the poor. The authors conclude that, although “concern about inequalities in maternal and child health in poor countries was conspicuously absent from the global agenda in the past,” the availability of new, intervention-specific data provides a means of targeting equity issues in health delivery more successfully. -
“Afghanistan, Against the Odds: A Demographic Surprise” Launches ECSP Report 14
›A few months ago, Elizabeth Leahy Madsen broke down Afghanistan’s first-ever nationally representative survey of demographic and health issues in a two-part series here on the blog. Now, we’ve published her analysis in a rich new policy brief format. It is the first issue of Environmental Change and Security Program Report 14, the latest volume of ECSP’s flagship publication.
In “Afghanistan, Against the Odds,” Madsen examines the surprising results of this fall’s demographic survey and how the country’s statistics compare to neighboring Pakistan.
“Just as Afghanistan and Pakistan’s political circumstances have become more entwined,” writes Madsen, “their demographic paths are more closely parallel than we might have expected. For Afghanistan, given its myriad socioeconomic, political, cultural, and geographic challenges, this is good news. But for Pakistan, where efforts to meet family planning needs have fallen short of capacity, it is not.”
The publication of this brief marks the re-launch of ECSP Report as an online-only volume, with individual issues scheduled to be released throughout the year. Forthcoming ECSP Report 14 briefs will address the demographic roots of the Arab Spring; the links between population dynamics and environmental resources like water, biodiversity, and food; and the potential impact of climate change mitigation efforts on conflict.
Published since 1996 in hard copy and online, the new ECSP Report will now be available on the Wilson Center website, New Security Beat, and Issuu. You can read the previous 13 volumes of the ECSP Report on the Wilson Center website.
Download ECSP Report 14: “Afghanistan, Against the Odds” from the Wilson Center. -
Adenike Esiet: Building Support for Improving Adolescent Sexual and Reproductive Health in Nigeria
›“In Nigeria, young people under the age of 25 are driving the HIV epidemic…and that’s been the opening place for people to begin to say, ‘let’s address the issues of young people’s sexual and reproductive health,’” said Adenike Esiet, executive director of Action Health Incorporated in Lagos, during an interview with ECSP.
On any number of health indicators, girls suffer disproportionately. “For every one boy in the age bracket of 10 to 24 who is HIV positive, there are three girls who are HIV positive,” Esiet said. “Over 60 percent of cases of complications from unsafe abortion reported in Nigerian hospitals are amongst adolescent girls. In fact in literature, 10-15 years ago, this was described as ‘a schoolgirl’s problem’…and it’s still an ongoing problem.” She added: “And for girls too, the issue of sexual violence is huge. It goes largely unreported but it’s occurring at epidemic levels.”
Esiet spoke on an adolescent health panel during the April 25 “Nigeria Beyond the Headlines” event at the Wilson Center. Progress is slow on these issues, in large part because “there’s a whole lot of silence about acknowledging young people’s sexuality,” she said.
Adults “want to believe [adolescents] shouldn’t be sexually active.” But turning a blind eye to adolescent sexuality can mean that efforts “to provide access to education or services is hugely resisted by practitioners who should be doing this.”
Action Health works to fill the gap that emerges. “Our work covers advocacy, community outreach, and service provision for young people,” said Esiet.
“Our primary entry road in to work with young people is creating access to sexuality education and youth friendly services. And in the course of trying to do that, we have to do a whole lot of advocacy with government and also with ministries or education and ministries of health and youth development.”
The group has worked with government officials and agencies to establish a nationwide HIV education curriculum and paired with local healthcare providers to increase access to “youth-friendly” sexual and reproductive health services. Funding shortages and insufficient resources have hampered the curriculum’s success, though, and the pervasive attitude against youth sexuality has limited the reach of services, she said. Ultimately, “there are a whole range of issues that truly need to be addressed” for outreach efforts to be successful.