-
To Reduce U.S. Maternal Mortality, Take Aim at Non-Communicable Diseases
April 8, 2020 By Wanda Nicholson
Every day there are more than 800 maternal deaths worldwide. Who are these women? They are reproductive women across the globe. They are our sisters, aunts, friends, and co-workers. They are leaders in our community, family members, and caregivers. When assessing the state of maternal morbidity and mortality in the United States, one must consider not only what we know, but also what must change.

Every day there are more than 800 maternal deaths worldwide. Who are these women? They are reproductive women across the globe. They are our sisters, aunts, friends, and co-workers. They are leaders in our community, family members, and caregivers. When assessing the state of maternal morbidity and mortality in the United States, one must consider not only what we know, but also what must change.
High U.S. Maternal Mortality Rate
While the United States has made progress in reducing maternal mortality, we also know that it is the only “high-resource” country that has not continued to substantially reduce mortality over the past decade. Women in the United States are much more likely to die in pregnancy and childbirth than women in other developed nations. The average maternal death rate in the United States in 2018 was 17.4 per 100,000 live births compared to a range of 5–9 per 100,000 live births in other high-resource countries.
A sobering fact is that black women are more than twice as likely to die compared to white women. In 2018, the Centers for Disease Control and Prevention reported 37.1 deaths per 100,000 live births in non-Hispanic black women compared to 14.7 deaths per 100,000 live births among non-Hispanic white women. Disparities in access to prenatal care, higher cesarean delivery rates, and a reduction in obstetrical providers in certain geographical areas are factors that contribute to maternal mortality. But we’ve been ignoring some other important factors. The reality is that we must broaden our focus to include non-communicable diseases. Specifically, we must note the growing rates of cardiovascular disease, obesity, and diabetes among childbearing women in the United States.
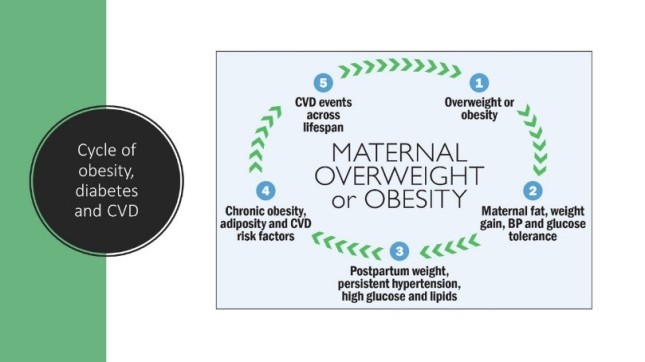
Cardiovascular disease is a leading cause of maternal mortality both domestically and worldwide. Recent data indicate that cardiovascular disease accounts for up to 27 percent of pregnancy-related deaths in the United States, with the majority of deaths due to coronary artery disease, postpartum cardiomyopathy, and congenital heart disease. Non-Hispanic black women are 3.4 times more likely to die from CVD-related conditions compared to white women, due in part, to disparities in care, institutional and systematic barriers, racial bias, and gender inequities. Coupled with the growing rates of overweight, obesity, gestational diabetes (also known as diabetes of pregnancy), and type 2 diabetes, it is clear that in order to combat maternal mortality, we will need to “break this emerging cycle” of chronic disease (Figure). Of the 4 million women who deliver each year in the United States, about 7 percent (~280,000) are diagnosed with gestational diabetes, with prevalence rates up to 10 percent in some regions. Obesity is a key risk factor for both gestational and type 2 diabetes mellitus and cardiovascular disease. In fact, about 60 percent of women are overweight or obese at the time of conception.
The threat of chronic, non-communicable disease to maternal health can be viewed within a cycle (Figure) of excessive gestational weight gain, hypertension, postpartum weight retention, persistent diabetes, and hypertension, with future risk of CVD events and a high-risk CVD profile.
Figure. Cycle of Maternal Obesity, Overweight, and Diabetes

What Must Change?
To reduce maternal mortality, we will need to take a comprehensive view of maternal and women’s health, including collaborative efforts in clinical care, integration of maternal social determinants of health, the life-course of women, and elimination of racial bias.
Collaborative Care
Efforts to break the cycle outlined above continue to draw attention to the need for early assessment of CVD risk factors, risk stratification based on the degree of risk followed by care from an interdisciplinary team to address CVD complications that may arise, and identification of risk factors for chronic disease and chronic disease prevention. Recommendations include establishing a low threshold for investigating cardiac symptoms both in pregnancy and postpartum, comprehensive evaluation using appropriate diagnostic tools, and most importantly, the development and deployment of transdisciplinary cardiac teams, including ob-gyns, maternal-fetal medicine physicians, anesthesia, and cardiology. The Society for Maternal Fetal Medicine and the American College of Obstetrician and Gynecologist have provided guidance for four levels of maternal care to respond to the range of conditions and care needed during the perinatal period. These recommendations outline the necessary clinical personnel and available healthcare services needed to meet each level of care. Because up to 30 percent of maternal deaths occur in the year after delivery, an extension of Medicaid and third-party reimbursement for postpartum care from 3 months up to one year could improve postpartum surveillance and reduce maternal deaths.
Racial Bias and Inequities
By 2050, people of color will represent the majority of the U.S. population. Yet, disparities across the spectrum of health care, including maternal care, persist. Racial bias and inequities in access and treatment among clinicians and the healthcare system must be addressed and eliminated. Racial bias can make it difficult to adequately assess maternal risk factors and identify at-risk women prior to, during, and after pregnancy. Often less than optimal patient-provider communication and providers’ misperceptions lead to unrecognized cardiac symptoms and gaps in intrapartum care and missed opportunities for early intervention in the postpartum period. It is critical to continue to acknowledge the impact of implicit and explicit bias in health and health care. Continued discussion and training of healthcare providers at all levels is essential to change provider behavior, enhance the maternal healthcare experience for women in all racial/ethnic groups, and improve patient outcomes. National medical organizations are joining in these efforts and committing to eliminating inequities in access and care.
Social Determinants Of Health
To further reduce maternal deaths, each of us will need to think more broadly about social determinants of health (SDOH)—the social context in which women live and work. In addition to racial/ethnic disparities, geographic and socioeconomic disparities contribute to the growth of chronic diseases. The World Health Organization released a report, Strategies toward Ending Preventive Maternal Mortality, to address issues related to poverty, inequality, and access to affordable health care. We must focus on innovative strategies to improve women’s health and well-being across their life course from birth to young adulthood, so that the years preceding pregnancy are prioritized in the same manner as pregnancy and the postpartum period. Integrating the life course model into the care of young women and girls may reduce the threat of non-communicable diseases, improve preconception, and ultimately birth outcomes.
Maternal mortality is a key indicator of a nation’s health and one measure of the health system’s response to maternal and newborn health and wellness. The contribution of CVD and its associated co-morbidities of obesity and diabetes to maternal mortality cannot be viewed narrowly. Rather, this cycle of chronic disease must be viewed with a broad lens that includes the healthcare system with transdisciplinary skilled teams; incorporates social and economic influences of where women live, work and raise their families into assessments of health and healthcare; and recognizes the life course approach. A maternal death has significant emotional and economic consequences for surviving offspring, partners/spouses, and families. Reducing maternal deaths and improving maternal care is critical to families now and for future generations.
Read More:
- Cardiovascular disease can be a silent killer during pregnancy and beyond.
- Mothers’ mental health erodes in Nairobi due to many stressors.
- Care for maternal health and non-communicable diseases must be integrated.
Wanda Nicholson, MD, MPH, is a professor in the Department of Obstetrics and Gynecology at the University of North Carolina at Chapel Hill. She previously served on the American College of Obstetricians and Gynecologists Presidential Task Force on Pregnancy and Heart Disease. Portions of this paper were presented at the launch of the Maternal Health Initiative’s CODE BLUE series at the Wilson Center on November 5, 2019.
Sources: American Medical Association, Centers for Disease Control and Prevention, Ethnicity & Disease, Maternal and Child Health Journal, Obstetrics & Gynecology, The American College of Obstetricians and Gynecologists, World Health Organization.
Photo Credit: Shutterstock.com, All Rights Reserved.
 A Publication of the Stimson Center.
A Publication of the Stimson Center.