Showing posts from category HIV/AIDS.
-
Jeanne Nyirakamana, PHE Champion
Reaching Rural Rwandans With Integrated Health and Livelihood Messages
›This PHE Champion profile was produced by the BALANCED Project.
Rwanda is one of the most densely populated countries on the planet, with more than 11 million people in one of Africa’s smallest countries, most of whom depend on the land as subsistence farmers. The country has diverse mountain, lake, and savannah landscapes, and the Virunga Mountain chain in the northwest part of the country is home to one-third of the world’s threatened mountain gorilla population. At the same time, the population throughout the country suffers from high rates of unmet need for contraception, and three percent of the adult population lives with HIV/AIDS. In a land under such intense pressure on natural resources, rural livelihood initiatives are critical to ensuring people have options for meeting their daily health and well-being needs.
For the past three years, Jeanne Nyirakamana has served as head of the health program for the Sustaining Partnerships to Enhance Rural Enterprise and Agribusiness Development (SPREAD) Project. Supported by the U.S. Agency for International Development through Texas A&M; University, the SPREAD Project is integrating a dynamic coffee production and quality improvement program in Rwanda with health outreach to improve community well-being. The health component works to improve the lives of coffee farmers and cooperative members by providing them with health information and services related to family planning, maternal and child health, prevention of sexually-transmitted infections (including HIV), and water and sanitation.
Training Peer Educators
Working closely with the coffee program, Nyirakamana’s team has trained more than 540 men, women, and youth peer educators who have reached more than 95,000 coffee farmers with education and services. Key communication messages highlight the links between sound decision-making and health-seeking behaviors, productive farms and agribusinesses, and strong and healthy families.
The program also leverages and supports local health resources through referrals to existing public health services, organization of mobile clinics, and community-based distribution of a socially marketed water purification solution (Sur Eau) and condoms (Prudence). According to Nyirakamana, one of the project’s greatest successes is the increased acceptance of family planning by farmers and their families and the more than 7,500 farmers who have been tested for HIV. In order to draw in as many coffee farmers as possible, many of the health and livelihood activities take place at the stations where the coffee beans are washed, at other buildings used by the coffee farmer cooperative, or during combined community meetings or home visits. At the washing stations, Nyirakamana’s team supports local health center staff to provide voluntary counseling and testing (VCT) and de-worming services while at the same time SPREAD-trained peer educators and coffee/health extension agents disseminate family planning information.
The cooperatives’ buildings have clean water, hand-washing stations, and small kiosks where condoms and Sur Eau are sold. These community health agents work with SPREAD to ensure that the greater community, not just the coffee farmers, has access to health knowledge and services. They learn how to teach the community about a range of health issues and each month they submit reports showing how many people they reached and with what kinds of messages. They are also becoming increasingly engaged in coffee and agribusiness activities. Through the success of their health activities, these agents are seen as vital community resources.
Integrated Results
By implementing this integrated population, health and environment (PHE) approach, the SPREAD Project staff is ensuring the health of the people and environment and success of the agribusiness. “You cannot care for the environment without first caring for the people who live and use that environment, so when you transmit dual messages [agriculture and health] you are able to hit two birds with one stone,” said Nyirakamana.
According to a 2010 evaluation of the project, farmers and their families reported improvements in personal and household hygiene; an increase in understanding and acceptance of family planning; uptake of HIV and VCT services; and use of condoms and other local health services. As well, they noted shifts in gender norms affecting household revenue use, alcohol, and reproductive health. The agribusiness stakeholders value the integrated approach as a means to more holistically meet farmers’ goals of increased incomes and improved lives and livelihoods.
This PHE Champion profile was produced by the BALANCED Project. A PDF version can be downloaded from the PHE Toolkit. PHE Champion profiles highlight people working on the ground to improve health and conservation in areas where biodiversity is critically endangered.
Photo Credit: BALANCED Project. -
Ben Ramalingam, Aid on the Edge of Chaos
The Complexity of Scaling Up
›October 11, 2011 // By Wilson Center StaffThe original version of this article, by Ben Ramalingam, appeared on Aid on the Edge of Chaos.
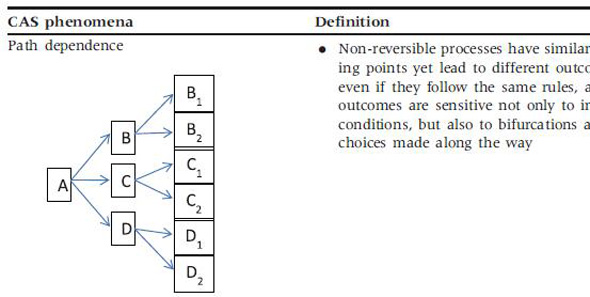
Despite increased prominence and funding of global health initiatives, attempts to scale up health services in developing countries are failing, with serious implications for achieving the Millennium Development Goals. A new paper argues that a key first step is to get a more realistic understanding of health systems, using the lens of complex adaptive systems.
Much ongoing work in development and humanitarian aid is based on the idea of “scaling up” effective solutions. Healthcare is one of the areas where this idea has played a central role – from the World Health Organization’s Health for All in the 1960s to UNICEF’s child healthcare programs, from rolling out HIV-AIDS, malaria and TB treatments to the package of interventions delivered to achieve the Millennium Development Goal on health.
However, despite the fact there are many cost-effective solutions to health problems faced in developing countries, many agencies are still frustrated in their attempts to deliver them at scale. This may be because of a widespread failure to understand the nature of health systems.
Continue reading on Aid on the Edge of Chaos.
Image Credit: Adapted from Table 1, “Understanding pathways for scaling up health services through the lens of complex adaptive systems,” Health Policy and Planning, Oxford University Press. -
Reporting on Global Health: A Conversation With the International Reporting Project Fellows
›“The story is the story, the information is the information, but you can frame it in very different ways,” said freelance journalist Annie Murphy at a roundtable discussion on the current state of global health reporting. Fresh off their five-week assignments, Murphy and three other fellows from the International Reporting Project (IRP) – Jenny Asarnow, Jill Braden Balderas, and Ann S. Kim – spoke at an event at the Woodrow Wilson Center on April 28 about their experiences researching underreported health issues in Haiti, Botswana, Mozambique, and Uganda. [Video Below]
Taking the Temperature of Global Health Reporting
Global health reporting, like many other forms of journalism, has felt the pinch from the global financial crisis, said Balderas, who edited a recent Kaiser Foundation report on the issue, “Taking the Temperature: The Future of Global Health Journalism.” Other challenges that have led to less global health coverage in mainstream media include an increased focus on “hyper-local” news; “story fatigue” from years of HIV/AIDS coverage; greater focus on epidemics and disasters; and the increasing number of advocacy groups starting their own news services.
Placing global health stories is a big challenge, agreed all four panelists. Who will want to run the story? What form – radio, documentary, print, online – will the story take? According to Murphy, some creative thinking may be needed: “It is global health, but that doesn’t mean we always have to frame it in this box of global health. It will be global health no matter what we do, so I think it’s also important for us to feed it into other events and issues that are important.”
(Re)building Maternal Healthcare in Haiti
With the worst maternal and infant mortality rates in the Western Hemisphere, Haiti needs medical providers of all kinds, said Asarnow, but especially skilled birth attendants. The devastating earthquake in 2010 destroyed Haiti’s only midwifery school, located in Port-au-Prince, killing many students and instructors. The school is still struggling to graduate a class of 15 people, she said.
In the rural town of Hinche, located in Haiti’s Central Plateau region, Asarnow frequently visited a public hospital that provided pregnant women with free obstetric care. Yet, she said, “even with free care, there [were] still a lot of barriers for women coming to the hospital to get care.” For example, the family members of expectant mothers had to provide sheets, clothing, food, and a bucket for personal needs. In addition, some women were too poor to afford transportation to and from the hospital.
Most women in Haiti, though, give birth at home with the help of traditional birth attendants, called matrones, Asarnow said. These matrones, popular in rural areas, are not formally educated in midwifery, but the government, along with non-profits such as Midwives for Haiti, have provided the matrones with training in basic health care and emergency situations.
Simply reporting on childbirth turned out to be a challenge, said Asarnow. “It’s hard to get people interested in something that just happens to most women,” she said; other more unusual health problems, such as infectious diseases, tend to garner more interest.
Finding Health Sovereignty in Mozambique
Health sovereignty, explained Murphy, is “the idea that nations have the right to make decisions about health and about how people are going to be treated” – an issue that is particularly pointed in Mozambique, where 50 percent of the national budget and 70 percent of the annual health budget is tied to international aid.
Mozambique, said Murphy, has only 1,000 doctors to serve a population of 22 million. By contrast, the country has an estimated 50,000 traditional healers. As a result, she said, most Mozambicans use traditional healing for at least part of their regular health care.
While researching traditional healers in the northern province of Tete, Murphy investigated a large Brazilian-owned coal mine that had displaced 5,000 local people when it was built. Mining is a major economic activity in Mozambique, yet mining companies are taxed a mere three percent by the government, said Murphy.
Health reporting doesn’t have to only cover traditional health issues, said Murphy. “The environment, natural resources, and how a country earns its money very much have to do with the health of the people who are living there,” she said. “How can you talk about being sovereign and providing health to your citizens if you don’t have the money to do that?”
Treating the Over-Treatment of Malaria in Uganda
“Malaria is quite over-treated” in Uganda, said Balderas. There’s the “idea that if you have a fever, you have malaria.” Consequently, the rate of misdiagnosis can reach alarming rates in some areas, she said.
Balderas said an estimated 50 percent of Ugandans get free treatment through the public sector. However, only donor-funded facilities are equipped with the rapid diagnosis test (or RDT), which takes only 20 minutes to determine the presence of malaria in a blood sample, she said. If these facilities were more widespread, misdiagnoses rates could easily be lowered.
Other challenges to the accurate diagnosis and treatment of malaria include faulty equipment, shortages of electricity and lab technicians, human error, corruption, bureaucratic entanglements, and presumptive diagnoses. For example, sometimes health workers do not know what is causing a patient’s fever, Balderas said, but they prescribe malaria treatments anyway because “they want to be able to give someone a treatment; they want to feel like they’re helping people.”
“There are certainly a ton of issues that relate to health,” Balderas said, such as poverty and corruption. Everyone she interviewed in Uganda – with the exception of government officials – identified the corruption in the country’s drug sector as a key problem.
Helping “Africa” One Small Story at a Time
Inspired by a World Health Organization study, which found “at least a 60 percent reduction in HIV infection among men who were circumcised,” Kim went to Botswana to investigate infant circumcision, a practice that is gaining popularity but is still alien. “I would meet people in the course of my day and they would ask me what I was doing there and I would talk about circumcision. They’d say, ‘Oh, I really want to get my baby circumcised. How do I do that?’” she reported.
The most powerful moment of her trip, said Kim, came when she was researching cervical cancer – the number one cancer among women in Botswana. As she waited with a woman to receive her lab results, Kim asked her if she was nervous. The woman, who was HIV-positive, said, “Yeah, I’m really worried. To me, it would be worse to get cervical cancer than to have HIV.” Even though Botswana is a middle-income country, said Kim, there are far more resources available to treat HIV than cancer.
Kim said that when presenting her work it was important for her to bring in the human element and not just the statistics: “I hope that, in whatever small way, even these small stories will help get issues in various countries on the map, especially in Africa where we tend to think of it as ‘Africa’ and not so much as different countries with different personalities and different situations.”
Sources: Malaria Journal, UNFPA, World Health Organization.
Image Credit: David Hawxhurst/Woodrow Wilson Center. -
Is Universal Access to Family Planning a Realistic Goal for Sub-Saharan Africa?
›“What do we require to ensure universal access to family planning services that are appropriate, affordable, accessible, and of good quality?” asked Michael Mbizvo, director of the Department of Reproductive Health and Research at the World Health Organization at the Wilson Center last month. [Video Below]
To talk about this difficult question and present research and programmatic evidence for sub-Saharan Africa, Mbizvo was joined by panelists Fred Makumbi, senior lecturer and head of the Department of Epidemiology and Biostatistics at Makerere University, Uganda; Oladosu Ojengbede, director of the Center for Population and Reproductive Health, University of Ibadan, Nigeria; and Frank Taulo, director of the Center for Reproductive Health and senior lecturer of obstetrics and gynecology at the University of Malawi.
Integrating Family Planning and HIV Services
Makumbi shared a number of findings on fertility preferences, behaviors, and contraceptive uptake in the context of HIV infection and care in Uganda. “Integrating family planning services into HIV services could help address the family planning needs of both HIV infected and uninfected,” he said.
According to new research conducted as part of the Rakai Community Cohort Study, despite significant gains in family planning use over time, there is still a high unmet need for contraception, irrespective of HIV status, in the Rakai district of central Uganda, said Makumbi. Male partner’s fertility desires were found to play an important role in pregnancy rates, and compared with previous studies conducted in the Rakai district, researchers saw an increase in pregnancy incidence and prevalence among HIV positive women, especially those on anti-retroviral therapy. HIV care that included voluntary counseling and testing was associated with significant increases in the use of family planning, and in particular, the use of condoms.
To effectively promote universal family planning in sub-Saharan Africa, “there is a need to strengthen family planning services in HIV care programs, with promotion of modern contraceptive methods, and with particular attention to women on anti-retroviral therapy,” said Makumbi. “Strategies to address desire for high fertility need to be developed, especially with regard to male involvement,” he added.
Multi-Pronged Approach to Universal Family Planning
“Family planning success in sub-Saharan Africa is a must for the region’s sustainable development,” said Ojengbede. “Poor commitment to women’s health in sub-Saharan Africa” has not only resulted in high fertility rates and poor maternal health indices but has also negatively impacted economic and human development in the region, said Ojenbede.
To increase access to and use of family planning, Ojengbede stressed the need to generate and sustain government commitment, promote legislation to support women’s autonomy, and implement policies to improve access to quality reproductive health services.
At the community level, Ojengbede said, the public health community must work to integrate family planning services into all reproductive health programs, including prevention of mother to child transmission; accelerate female empowerment programs; actively engage males in family planning access and uptake; and address social and cultural barriers that prevent widespread adoption of family planning.
“Traditional rulers can occupy a critical position to enact positive change in their communities and at the national level,” said Ojengbede. In Nigeria, for example, providing education about the health and economic benefits of family planning has helped traditional leaders embrace family planning and develop their own strategies to promote birth spacing in their communities.
“Universal family planning access must be achieved through a multi-pronged approach that should be colored with socio-cultural sensitivity, solid evidence, and sustainability,” concluded Ojengbede.
Eliminating Unmet Need: “Yes, We Can”
“It is time to prioritize issues that are affecting women and family planning is a very critical area,” said Taulo.
There are still many challenges to overcome before Malawi can achieve universal family planning access, including poverty, misconceptions and myths about family planning, lack of availability of reproductive health supplies, poor infrastructure, shortage of trained professionals, and religious and cultural barriers.
“Commodities are also very much dependent on the donor,” said Taulo, pointing to the challenges of insufficient funding and political will. “Failure to connect family planning to economic development and political stability is one of the main areas that we are struggling with,” he added.
“We have lots of challenges, but also many achievements,” said Taulo. Malawi has made important strides in expanding access to family planning by implementing community-based strategies and youth-friendly programs, developing public-private partnerships, engaging policymakers and traditional leaders, and encouraging media coverage of family planning issues.
“Education is another family planning product,” said Taulo. Moving forward, a “deliberate focus on girl child education” and promotion of women’s welfare can have a major impact on fertility reduction, he said.
“We can eliminate unmet need for family planning in Malawi, if we put our heads together, our thoughts together, and our energy together,” concluded Taulo.
Source: World Health Organization.
Image Credit: “Women’s Health Clinic” courtesy of flickr user advencap. -
The Role of Population Dynamics in Climate Adaptation
›December 21, 2010 // By Wilson Center StaffThis post is a synthesis of a panel discussion at the UNFPA Population Dynamics and Climate Change conference in Mexico City with Marcia Castro, of the Harvard School of Public Health; Heather D’Agnes, of USAID; and Lori Hunter, of the University of Colorado at Boulder.
It is well-known that environmental change — including climate change — has important impacts on human health. However, it is less well understood how health systems shape the responses of individuals and households to environmental change. Population dynamics — such as fertility, migration, and mortality and morbidity — influence community health and greatly affect community resilience in the face of environmental changes, including the capacity to adapt to climate change.
Mortality and Morbidity
Morbidity and mortality dramatically shape a household’s ability to adapt its livelihood strategies to a changing climate. For example, in areas of high HIV prevalence, such as sub-Saharan Africa, adult mortality seriously undermines livelihood options. In the face of such loss, the household’s reliance on local natural resources intensifies. If environmental change reduces the amount of available resources, the household has fewer options for energy and sustenance.
Morbidity also affects adaptive capacity, and morbidity itself can be shaped by environmental change. For example, environmental scarcity can increase poverty, which can lead to an increase in risky transactional sex, further fueling the HIV pandemic. Malnutrition resulting from drought and environmental shocks can suppress the immune systems of HIV-positive people, making them more vulnerable to illness and less able to adapt to other external changes.
Fertility and Family Planning
Healthier households are more resilient households, so increasing access to health services, including reproductive health services, is essential for building adaptive capacity. High fertility poses challenges to a family’s livelihood and has negative health effects on women and children. Providing reproductive health services is an effective way to improve the capacity of these vulnerable groups to adapt to climate change. For example, a recent study argues that lowering fertility rates in the Himalayan region could increase community resilience to the predicted fluctuations in water quantity.
However, there is a high level of unmet demand for contraception across the globe. How can community adaptation programs help meet this need? Importantly, research from the Philippines suggests that integrating population, health, and environment programs in a package approach to community development is more effective than single-sector interventions. Including family planning and reproductive health services in community-based climate adaptation programs could not only more effectively meet the community’s needs, but could also improve its adaptive capacity better than health or climate programs alone.
Migration
Another population process, migration, can both impact health and affect the capacity for adaptation. For example, internal migration in the Brazilian Amazon appears associated with the spread of malaria, which negatively impacts the adaptive capacity of households. To mitigate climate change’s health impacts, states should more effectively plan settlements and health systems, including health impact assessments for infrastructure and development projects. (Editor’s Note – northern Nigeria and Niger present another example of similar climate-related migratory patterns that significantly impact health and economic resilience.)
In summary, the scientific evidence is clear that population dynamics — such as mortality, fertility, and migration — and environmental trends are linked. Projects intended to improve a community’s ability to adapt to a changing climate should consider and address these linkages in their design and implementation.
Sources: Foundation for Environmental Conservation, UNFPA, USAID.
Photo Credit: “Toureg family in Niger,” courtesy of flickr user ILRI. -
Expanding Access to Maternal Health Commodities
›“This is not just about getting quantities of drugs out, this is about saving women’s lives with really simple products that work,” said Julia Bunting, team leader of AIDS and reproductive health at the UK Department for International Development and coalition chair of the Reproductive Health Supplies Coalition, at the ninth meeting of the Global Health Initiative’s 2009-2010 Advancing Policy Dialogue on Maternal Health series. Joined by panelists Melodie Holden, president of Venture Strategies Innovations (VSI), and Elizabeth Leahy Madsen, senior research associate at Population Action International (PAI), the panel discussed the challenges and strategies for expanding access to maternal health commodities.
Integrating Maternal Health and Family Planning Supply Chains
“It is often said that the family planning and the maternal health communities have very different views of supplies… but actually [both communities] recognize that we need to explore the continuum,” said Bunting, addressing the need to integrate maternal health commodities into existing reproductive health supply chains. “I really think the stars are aligned right now for advancing this agenda,” added Bunting.
“Many of the commodities that we talk about in terms of reproductive and maternal health cost tiny amounts to deliver, but actually save lives and are some of the most cost-effective interventions we have both in public health and in broader development,” said Bunting.
No Product, No Program
“Supplies are a key element in programs to improve maternal health and they are also a tangible and visible hook to increase awareness and commitment,” said Madsen. “Policymakers whose eyes glaze over when they hear the term ‘health systems strengthening’ can grasp… much better when they learn that supply shelves in clinics are bare and that women are making great efforts to reach facilities, only to leave empty- handed,” said Madsen.
Presenting research conducted by PAI, Madsen discussed the availability of four key maternal health medicines and products in Bangladesh and Uganda including:
By focusing on supplies that target the three leading causes of maternal mortality, Madsen and her colleagues identified factors that inhibit access to these commodities and developed recommendations for strengthening maternal health supply chains.- Oxytocin: used to prevent post-partum hemorrhage
- Misoprostol: used to prevent post-partum hemorrhage
- Magnesium Sulfate: used to treat pre-eclampsia
- Vacuum Aspirators: used for treatment of early and incomplete abortion
Madsen identified several strategies to strengthen supply chains for maternal health commodities including forecasting and preparing for growing demand, advocating for government and donor support, encouraging scaling-up of community-based approaches, promoting family planning, and focusing on human resource training.
“In maternal health, if a supply to prevent or treat a life-threatening complication is in stock, there must also be a way for a woman to reach it in time… and in most cases a provider who knows how to administer it,” said Madsen.
“This research is intended to lay the groundwork for future advocacy and policy initiatives by providing an evidence base that is informed by local expertise,” said Madsen. “We hope that this information will inform program implementation, funding decisions, and awareness raising.”
Getting the Product to People: The Case of Misoprostol
“The story of Misoprostol is still being written. The goal is to invest in creating access to interventions that are low-cost and relatively simple to use,” said Holden. By sharing lessons learned, Holden described VSI’s experience registering and procuring Misoprostol and demonstrated how community mobilization is imperative to overcoming major challenges for large-scale implementation.
“Making products available is not without challenges,” said Holden. To increase access to Misoprostol in rural communities, maternal health experts must work to “engage communities, educate and mobilize women, train providers at all levels of the health care system, and provide support to distributors to jump start sales,” said Holden. “By looking holistically across entire health systems, bringing in great interventions, addressing the components of supply and demand, and working with local partners, we can have lasting impact.”
While the price of Misoprostol has decreased significantly, Holden stressed the need to identify creative ways along the supply chain that reduce costs to the end user. Additionally, “establishing policies around this new intervention not only establishes its reach, but also makes its use institutionalized, which means it will be part of the system even if governments or individuals change,” said Holden.
“If there is a gap between what could be achieved with Misoprostol and what is being achieved, we need to go back to the model and figure out what pieces aren’t working,” concluded Holden. “The work is complex and takes time, but it’s worth it.”
Photo Credit: “Rapid HIV testing,” courtesy of flickr user DFID – UK Department for International Development. -
World AIDS Day 2010: Not Yet in a Position to Say “Mission Accomplished”
›December 1, 2010 // By Schuyler NullToday is World AIDS day. More than 33 million people are currently living with HIV around the world, according to the UN, and the vast majority of them (22 million) are located in sub-Saharan Africa.
“We have halted and begun to reverse the epidemic. Fewer people are becoming infected with HIV and fewer people are dying from AIDS,” said Executive Director Michel Sidibé in the 2010 edition of UNAIDS’ annual report.“However we are not yet in a position to say ‘mission accomplished.’ Growth in investment for the AIDS response has flattened for the first time in 2009. Demand is outstripping supply. Stigma, discrimination, and bad laws continue to place roadblocks for people living with HIV and people on the margins.”
Particularly in sub-Saharan Africa, “people on the margins” often means women and children. As a result, there has been more and more integration of HIV/AIDS programs with gender and maternal health. The environmental community has also worked closely with HIV/AIDS interventions in places where the destruction of natural resources makes certain populations more vulnerable than others and valuable conservation efforts are threatened.
As development efforts become more cross-sectoral, it’s important to keep in mind and maximize these connections between community, economic, and environmental health.
Check out The New Security Beat’s coverage of HIV/AIDS integration with other health and environment programs including coverage from the Global Health Initiative’s “Integrating HIV/AIDS and Maternal Health Services” event last year, a sit-down interview on the challenges facing HIV-positive adolescents with Harriet Birungi of the Population Council in Kenya, and an examination of how gender-based violence contributes to women’s vulnerability to HIV.
Sources: Population Reference Bureau, UN, World Wildlife Federation.
Map Credit: World AIDS Campaign. -
PRB’s Jay Gribble at Kenya’s National Leaders Conference on Population and Development
›November 29, 2010 // By Wilson Center StaffJay Gribble, vice president of International Programs at the Population Reference Bureau (PRB), recently attended the Kenya National Leaders Conference on Population and Development, November 15-17, at the Kenyatta International Conference Center in Nairobi. During the conference, he produced a series of posts for PRB’s Behind the Numbers on some of his impressions. Gribble focuses on Kenya’s resurgent interest in integrating population issues into the development agenda, the country’s ongoing HIV/AIDS epidemic, and the importance of family planning.
Below are the introductory excerpts from his posts; to read the full posts, please visit Behind the Numbers.
“Anticipating Change in Kenya”
Sitting in the hall where Kenya’s National Leaders Conference will be starting in a few minutes, I can’t help but feel that there is an opportunity to refocus national attention to development…to the goal that I have heard repeatedly of becoming a Middle Income country. And to achieve this goal, they must first recognize that population is an underpinning development issue that cannot be ignored.
In the 1980s and 1990s, Kenya was a leader in reproductive health and maternal health, really setting a pace for the continent. But during the 2000s, Kenya turned its attention to other pressing issues – namely HIV/AIDS – and began to give less attention to population issues. Though HIV continues to be a plague, it is now time to return to the importance of slowing population growth, for until this fundamental issues is addressed, there will be less opportunity for education, jobs, and better health. At the same time, as a predominantly rural country with agriculture representing a major part of the economy, smaller families will be critical to maintaining farms that are large enough to feed families and the country.
Continue on PRB.
“As the Rich Get Richer, the Poor Get Children”
The Kenya National Leaders Conference has begun, representing the first time since 1989 that Kenya’s national population policy has been discussed in a large, open forum. With a new national constitution, Kenya is poised to redress many of the social and economic inequalities that have stood in the way of its development. In fact, the current population policy expires in December, 2010, and one of the purposes of this conference is to gather the input from leaders throughout the country on how a new policy should be framed. I find it impressive that such a large conference is convened to ensure that a new policy reflects the needs of the nation. The conference is also a forum for reaching leaders with important information about the need to address population growth through family planning if Kenya is to achieve its Vision 2030 development plan.
Continue on PRB.
“In Kenya, Prioritizing Population…and Family Planning”
As Kenya’s National Leaders Conference on Population and Development winds down today, it offers leaders an opportunity not only to think and talk about how population growth is an issue that underlies the country’s development, but to act on it too. Whether thinking about business, agriculture, or the environment, it is impossible to be strategic about Kenya’s future without also considering how rapid population growth will affect it.
In talking with Kenyans who grew up in the 1970s and 1980s – back when family planning and population growth were a priority – they remember the messages that were at the tips of people’s tongues – smaller families live better. Before the HIV/AIDS epidemic, family planning and slowing population growth was a priority and a source of national pride because it put Kenya on track for prosperity and development.
Continue on PRB.
Photo Credit: Adapted from “King Kenyatta?” courtesy of flickr user rogiro.