-
Sustaining PEPFAR’s Success through Integration, Equity, and Inclusion
April 19, 2023 By Deekshita Ramanarayanan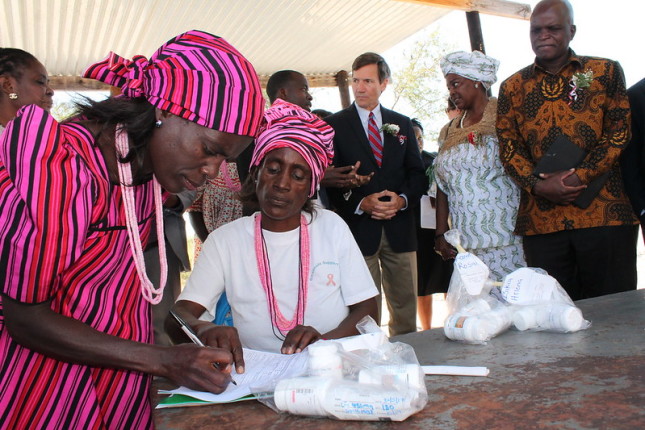
It has been two decades since President George W. Bush launched the U.S. President’s Emergency Plan for AIDS Relief – or PEPFAR, and a recent Wilson Center event to celebrate the anniversary demonstrated that its impact as one of the most successful global public health programs is indisputable. Since its inception, PEPFAR has invested more than $100 billion in the global fight against HIV and AIDS, resulting in more than 25 million lives saved and millions of new infections prevented.
“Over the last 20 years, this bipartisan program has changed the course of human history in so many ways,” said Ambassador Mark Green, President and CEO of the Wilson Center, who co-authored the initial legislation that created PEPFAR when he served in the House of Representatives.
“[PEPFAR] has entirely transformed our collective understanding of what is possible for incurable viruses and global health,” said Beirne Roose-Snyder, Senior Policy Fellow at the Council for Global Equality.
This year, Congress will deliberate on the reauthorization of PEPFAR for the fourth time since its inception. Reauthorization is a critical part of sustaining PEPFAR and encouraging other countries and global donors to invest to reach the 2025 targets and to end the epidemic by 2030, said Vinay Saldanha, Director of the U.S. Liaison Office at UNAIDS.
“There’s so much that can be done within the legislation that currently exists and so much opportunity for forward movement,” said Roose-Snyder.
Filling a Key Gap
In the absence of an HIV vaccine or cure, reducing new infections relies on the implementation of evidence-based prevention programs, such as those supported by PEPFAR, said Saldanha. Today, more than 20 million people globally receive life-saving antiretroviral treatment (ART) to treat the HIV infection. “This is an increase of not 300 percent, but 300-fold, or 300 times, since 2004,” he said.
Further, new HIV infections and deaths in sub-Saharan Africa, the regional priority of PEPFAR programs, have decreased by half since 2003. “What is clear from all the data that UNAIDS collects on an annual basis is that the progress in countries with the greatest reductions in HIV infections is happening precisely because they’re supported by PEPFAR,” said Saldanha.
He also pointed to PEPFAR’s positive “spillover effects,” including a 35 percent reduction in child mortality, a nine percent reduction in girls and boys leaving school, a ten percent increase in immunizations, and a 2.1 percent increase in global GDP per capita. PEPFAR has changed the landscape of how the world addresses global health challenges, such as tuberculosis (TB), Ebola, mpox, malaria, and COVID-19.
“There are millions of people, including many marginalized and vulnerable people who have access to prevention services and treatment today because of both the vision and the execution of PEPFAR,” said Roose-Snyder.
Providing HIV Services in Fragile Settings and the COVID-19 Pandemic
Whenever there is a humanitarian crisis, be it natural or man-made, one key pillar of PEPFAR is ensuring continuity of services. “To be honest, with crisis and shocks, you never predict it,” said Dr. Joram Sunguti Luke, HIV and AIDS & Sexual and Reproductive Health and Rights (SRHR) Technical Advisor at Pathfinder in Kenya. Nobody predicted the catastrophic impacts of the COVID-19 pandemic, he said.
During the pandemic, PEPFAR programs made several adaptations such as multi-month dispensing and decentralized distribution of prevention and treatment services to ensure continuity of care. Programs were able to utilize and adapt the infrastructure in place for infection prevention and control of HIV and TB to provide testing and treatment for COVID-19. Dr. Luke added that repackaging the technical guidance on providing services during the COVID-19 pandemic to guide the HIV response in humanitarian responses beyond COVID-19 would strengthen PEPFAR in humanitarian settings.
COVID-19 created an obstacle that kept pregnant and breastfeeding mothers coming to clinics to receive maternal and child health services, said Rosemary Njogu, Senior Program Lead at Jhpiego in Kenya. She noted that the interaction between COVID-19 and HIV was “very unclear,” causing some women to avoid seeking care due to fear of transmission of COVID-19. Pregnant and breastfeeding women feared that living with HIV or having a high risk of HIV infection would make contracting COVID-19 a death sentence. Many girls who were sent home from school during the pandemic did not return at all, increasing their risk of experiencing gender-based violence (GBV) and their risk of HIV infection, said Njogu. She added that health workers in PEPFAR-supported clinics faced additional burdens as clinics were receiving instruction to divert resources away from HIV and AIDS services to focus on the COVID-19 pandemic.
Integration of Care to Reach Women and Girls
“Women and girls continue to account for the majority of new HIV infections in sub-Saharan Africa, and this makes HIV prevention and treatment a really critically important part of reproductive and maternal health care,” said Valerie Percival, a Wilson Center fellow and the moderator of the event.
Investments in prevention of mother to child transmission of HIV (PMTCT) resulted in 5.5 million infants born HIV-free in 2021. However, pregnant and breastfeeding mothers continue to face barriers in accessing safe and stigma-free services, particularly when they are living with HIV, have experienced GBV, or live in low-income areas.
Integrating HIV services in maternal health clinics and training health workers to provide stigma-free care increases the likelihood that pregnant and breastfeeding mothers will access HIV prevention and treatment services. Njogu and her team leveraged PEPFAR funding to integrate ART provision in maternal and child health clinics after noting that only 60 percent of pregnant and breastfeeding mothers were receiving treatment for HIV through referrals to other clinics. “And this is where we saw what was the biggest game changer,” she said.
Interventions to healthcare workers on respectful maternity care, the implementation of evidence-based models such as group antenatal care, and scaling up prevention services are critical to reach women and girls to “sustain the gains” achieved thus far, said Njogu. Programs such as DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe) have allowed girls to thrive in their communities and families, she said. The success of DREAMS also shows that services can be integrated to address behavioral and structural factors that increase the risk of HIV infection, said Dr. Luke.
Inclusion of Marginalized Groups to End the HIV Epidemic
In 2021, 70 percent of new cases of HIV were among key populations, which includes men who have sex with men, transgender people, female sex workers, and people who inject drugs. “There is simply no way to end the HIV epidemic without key populations,” said Roose-Snyder.
Yet a key challenge is that these classifications often intersect, she continued. For example, transgender people may be pushed into informal work, including sex work, because of social exclusion and stigma. “They are at best stigmatized, and at worst criminalized. That criminalization drives the epidemic, not individuals,” she emphasized.
Twenty years after the initiation of PEPFAR, criminalized and stigmatized groups are being given the opportunity to serve their own communities in PEPFAR programming; however, many governments globally do not prioritize key populations or invest in their safety. In fact, some governments, most recently the Ugandan Parliament, are actively targeting key populations.
It is imperative that PEPFAR place the service provision and leadership for key populations at the center of the HIV response moving forward, added Roose-Snyder. This involves increasing engagement with key populations and civil society in the decision-making process for PEPFAR—such as in Country Operating Plan meetings—while ensuring their safety. Building capacity within these groups allows them to set the standard for their care, create sustained change, and advocate for investment in interventions they have organized and support, she said. “We cannot continue to treat the human rights of key populations as a side story.”
Sources: Kaiser Family Foundation, National Institutes of Health, Reuters, United States Agency for International Development, United States Department of State.
Photo Credit: Namibia’s Onyaanya-Gwaanaka Refill Group distributing ARV community members. Photo courtesy of USAID in Africa.
 A Publication of the Stimson Center.
A Publication of the Stimson Center.



