-
Integrated Health Security Depends on Primary Health Care—and Engaging Men
April 26, 2023 By Daniel Shodell
USAID’s primary health care (PHC) partnership—which was announced in late 2022—brings new momentum to a long-neglected reality: Robust PHC is necessary for robust global health security (GHS). But it has taken some time to fully recognize this fact.
In 2018, the Lancet Commission explored synergies between universal health coverage, health security, and health promotion, finding that the key barrier was fragmentation of efforts, with complementary activities pursued through overly narrow mandates. Failures in COVID-19 response have provided the impetus to rediscover and redress this barrier. Meaningful support of PHC for health security is emerging, and a major inflection point is at hand.
The USAID Accelerating Primary Health Care Collaborative, with its focus on seven countries, can lead the way. But this effort must be intentional—and move beyond the agency’s historical focus on women and children to include men as both change agents and clients.
By shifting their paradigm to be fully inclusive and comprehensive, USAID can strengthen health security by pushing for a greater involvement for men while simultaneously improving reproductive and maternal child health services. Such a change may even create momentum for a shift in definitions of health security, and establish a new term for it: Integrated Health Security.
Primary Heath: Foundation for Transformation
An approach focused on PHC is critical for health security in multiple ways.
First, of course, there is proximity. Community-based service delivery is the main point of contact most people have with the health system, and it serves as a principal conduit for localized, trusted information during a health emergency. Primary health care also improves community health and reduces susceptibility to illness (e.g. through immunization), and provides health services when inpatient facilities are overwhelmed.
Primary health care also can provide some of the earliest signals of emerging health issues through front-line public health surveillance. It is difficult to conceptualize effective pandemic preparedness, prevention, detection, response, and recovery without the linchpin of PHC, especially in remote and underserved areas.
Nonetheless, PHC remains absent from both the International Health Regulations (IHR) and the Global Health Security Agenda (GHSA). This gap has been increasingly recognized, however. Substantive PHC mentions now can be found in IHR reform efforts; the pandemic treaty draft; and WHO’s proposal for strengthening the health emergency preparedness, response, and resilience architecture.
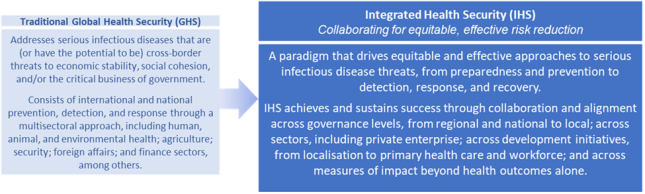
Not only are these developments promising, but they may also signal the emergence of a new paradigm to set the stage for better connecting PHC and health security. Palladium is proposing a name for this new paradigm: Integrated Health Security (IHS). Contrasted with traditional global health security (see figure), IHS reflects the driving forces that have brought PHC into these discussions.

The traditional concept of GHS emerged with a focus on protecting high-income countries from infectious disease threats, regardless of the high burden and limited benefit for low- and middle- income countries. Yet IHS answers the important question of “security for whom?” with an emphasis on collaboration and equity, and reflecting the principles that are foundational for connecting PHC to health security.
Integration in the context of IHS refers to geography and governance levels (moving beyond global and national to regional and subnational activities), multisectoral engagement with renewed emphasis on private sector (especially in context of PHC service delivery, as well as strengthening One Health across human, animal, and environmental sectors), and alignment with sustainability and localization initiatives.
Finding the “Missing Men”
Primary health care is a foundational element of IHS. And while the momentum building towards meaningful support of PHC for health security is welcome, it is notably being driven by international multi-lateral bodies.
In the United States, the story is a bit different. While we wait for an update of the 2019 health security strategy, the 2022 National Biodefense Strategy does include a section on “Achieving Global Health Security.” Yet this inclusion remains narrowly oriented around current IHR and GHSA practices, which do not encompass primary health care. The State-USAID Joint Strategic Plan likewise does not include PHC, and focuses health on services for women, youth, and marginalized groups.
In this context, the USAID PHC partnership may be perceived as having limited relevance to health security, and warrants some level of concern that the emerging focus may mirror USAID’s ongoing priorities to serve primarily women and children. This approach would fall far short of the PHC partnership’s potential to strengthen health security. USAID should recognize that the same barriers the Lancet Commission flagged in 2018 are a specific threat to full success of the PHC partnership.
Currently, and in keeping with long-standing history and practice, USAID focuses on family planning (FP) and reproductive, maternal, newborn, and child health (RMNCH). Services for men have been mainly oriented around their role as gatekeepers, rather than clients, although this balance may be slowly changing, in particular for HIV services through PEPFAR. Yet there is now a powerful opportunity to move beyond these silos and realize the full potential of PHC, while still improving benefits to FP/RMNCH.
Engaging men also can be an important factor in improving services for women and children. Evidence has demonstrated the role of men in strengthening FP access. The engagement of men in RMNCH also has shown health benefits for women and children. Beyond this, men are an integral link for any momentum toward IHS. Men need access to vaccination, the opportunity to connect with a local source that can be trusted for accurate risk communication, and they are critical participants in outbreak response to reduce disease transmission.
But engaging men in PHC and strengthening IHS requires seeing men as clients themselves—and not merely gatekeepers. This shift in perspective does not diminish the inequities that women and children face, nor does it ignore the disparities in health care access and outcomes that drive high rates of maternal and child morbidity and mortality. Any discussion of these issues must be framed in the broader context of gender inequality that impacts women, and cultural norms that prioritize services for men over those of women and children.
Yet as we have noted, there is growing evidence that engaging men can strengthen FP/RMNCH, improve baseline community health (decreasing susceptibility and increasing resilience during the next health emergency), and provide stronger platforms for delivering population-wide medical countermeasures, including immunization. Just as important, this engagement can reach all community members—young, old, men, and women— with a local source of health information that can be a trusted source for information as infectious disease threats emerge.
Decades of vertical initiatives have revealed the “missing men.” The PHC partnership will be among the first opportunities for USAID to expand its focus and make a true community-wide approach operational. The new PHC partnership can boldly drive gains across both FP/RMNCH and IHS, improving community health and expanding readiness for the next infectious disease threat. To achieve this, USAID and the initial PHC partnership countries should be intentional, explicit, and ambitious in their aim to engage—and integrate—men.
Daniel Shodell, MD, MPH is a public health physician and Integrated Health Security advisor for Palladium
Sources: Gates Open Research; International Journal for Equity in Health; PLOS one; The Lancet; Political Studies; USAID; The White House; World Health Organization.
Photo Credit: Angolan community members at HIV/AIDS outreach event. Credit: USAID.
 A Publication of the Stimson Center.
A Publication of the Stimson Center.