-
Covid-19 // Dot-Mom // Guest Contributor
Maternal Health and The Pandemic: It’s Not Good News
January 4, 2023 By Adrienne Griffen
COVID-19 has dealt out a double dose of woe for global maternal health. According to a new report from the Government Accountability Office (GAO), the pandemic saw an increase in maternal deaths and an exacerbation of racial disparities driving this overall morbidity. In addition, childbearing people experienced significant anxiety and depression.
Maternal mortality refers to the death of a woman during the perinatal period, which includes pregnancy, delivery, and the first year following pregnancy. Prior to the pandemic, approximately 700 women died each year during the perinatal period, making the United States one of the most dangerous high-income countries in which to give birth. Not only is our nation’s maternal mortality rate (the number of deaths per 100,000 live births) increasing, but it is also the highest of any high-income country. Significant racial and ethnic disparities exist as well, with Black women dying at 3-4 times the rate of white women. These concerns spurred the White House to publish a Blueprint for Addressing the Maternal Health Crisis in June 2022, created with the ambitious goal of making the United States the “best country in the world to have a baby.”
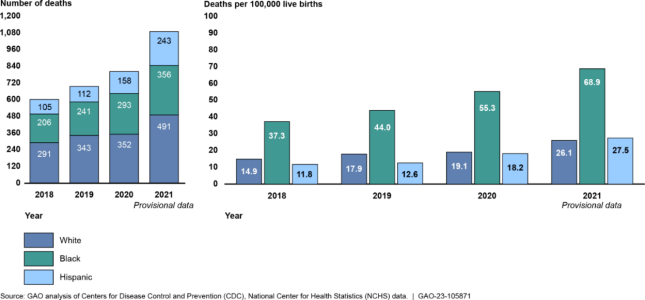
The new evidence on offer is particularly unwelcome as the next Maternal Health Awareness Day approaches on January 23, 2023. The GAO report shows that the overall number and rate of maternal deaths increased during the COVID-19 pandemic, Black women continue to die at significantly higher rates than their white counterparts, and the maternal mortality rate for Black birthing people almost doubled from 2018 to 2021.
Maternal Mortality During the Pandemic
The new statistics offered by the GAO state that the number of maternal deaths increased by 35 percent during the pandemic (from 754 deaths in 2019 to 1,178 deaths in 2021). This increase was fueled by COVID-related deaths, which accounted for 25 percent of maternal deaths in 2020 and 2021 combined. If not for these COVID-related deaths, the maternal mortality rate would have remained virtually unchanged.
Digging deeper into the data shows that race and ethnicity were important factors in the increase in maternal mortality during the pandemic, with Black and Hispanic mothers being disproportionately impacted [The GAO report only included data for Black, Hispanic, and white women.] While these disparities have long existed, they were exacerbated during the pandemic: the number of deaths for Hispanic women more than doubled (from 105 to 243), and the maternal mortality rate for Black women rose from 37 to almost 70 deaths per 100,000 live births. (See chart below).

Why Did So Many Mothers Die?
According to the Centers for Disease Control and Prevention (CDC), basic physiological factors – such as decreased lung capacity and/or a weakened immune system – may have left pregnant people more susceptible to the coronavirus. The Delta variant, in particular, significantly increased the number of deaths for pregnant people compared to before the pandemic.
The pandemic also compounded certain social factors that contribute to disparities in maternal health outcomes. The GAO report concludes that social determinants of health—where people are born, live, learn, work, play, worship, and age—along with racism and bias in the healthcare system combined to fuel the increase in deaths among Hispanic and Black women, especially those living in low-income neighborhoods. These women were likely to live in more crowded homes, meaning they were not able to maintain safe social distancing; to have challenges in accessing the internet or having privacy, meaning they were not able to fully utilize telehealth services; to be essential workers in the care-giving or service industries, meaning they could not work from home; and to face significant challenges in getting time off from work or finding childcare, meaning they had additional barriers in accessing healthcare.
A lack of transparency in communication also played a role. Frequently changing guidance and a lack of information (or misinformation) about COVID-19 early in the pandemic increased mistrust in the healthcare system among pregnant people, especially those from low-income or racially-diverse populations.
Maternal Mental Health and the Pandemic
Rates of maternal depression and anxiety also increased during the pandemic. Questions and concerns were widespread, especially early in the pandemic, leading pregnant women and new mothers to worry about things birthing people didn’t need to consider prior to the crisis, including fears of infection, being isolated from family support, and concerns about breastfeeding and infection spreading.
Newborns (and their parents) are usually the center of attention, with friends, family, and neighbors visiting with gifts and meals. During the pandemic, new parents often found themselves isolated and alone.
The infant formula shortage that occurred in the spring and summer of 2022 added more stress and anxiety to new parents. A work colleague who was expecting her second baby told me that she was so anxious about having enough formula that she had relatives in several states purchasing formula at ever-increasing prices. When I talked with her again recently, and she said her anxiety continues (her baby was born in August) because baby formula is being rationed. It is shocking that in the richest country on earth that new mothers are worried about how they are going to feed their infants. How is it possible that in the United States – the richest country on earth – that new mothers are worried about having access to necessary food for their infants?
Better Progress on Bellwethers
Maternal mortality – and its sister statistic, infant mortality — are widely considered to be bellwethers of the health and welfare of a country, representing the effectiveness of a nation’s healthcare system. We must do better – such as extending pregnancy-related Medicaid coverage to a full year postpartum and screening and treating maternal mental health – to ensure that new mothers and their infants get off to the best start possible. It is a resolution well worth making as the calendar turns to 2023, and the long-term impacts of the pandemic continue to ripple through our public health infrastructure—and society at large.
Adrienne Griffen is the Executive Director of Maternal Mental Health Leadership Alliance, a national nonprofit focused on policy and advocacy for maternal mental health.
Sources: Kaiser Family Foundation, Maternal Mental Health Leadership Alliance, Seminars in Perinatology, The Commonwealth Fund, The White House, United States Centers for Disease Control and Prevention, United States Department of Health and Human Services, United States Government Accountability Office
Photo Credit: Belly of pregnant woman. Evgeny Atamanenko/Shutterstock.com
Note: Although not all childbearing individuals identify as women, I will use the terms “women” and “mothers” in keeping with the terminology in the GAO report.
 A Publication of the Stimson Center.
A Publication of the Stimson Center.