-
Creating a New Normal with a New Global Public Health System
April 7, 2021 By Frederick M. Burkle
“Ask a big enough question, and you need more than one discipline to answer it,” said modern dance legend Liz Lerman.
As the COVID-19 pandemic spread across the globe, the World Health Organization (WHO) warned that there would be no going back to normal. They knew a failure to make timely and accurate public health decisions for a pandemic would prove to be the “difference between life and death.” How correct they were.
The problem: Global pandemics without a global public health management system
In the early stages of COVID-19, major public health decisions in the United States for prevention and preparedness were not made by public health experts. Instead, the experts were systematically ignored, removed, and taken over by political and economically driven decision-makers. Because of this, at the outset of the pandemic, traditional hospital and community-based health providers—trained to diagnose and manage individual patients—were increasingly faced with rapidly emerging and widely expanding public health and triage decisions that impacted large populations well beyond their local community. Population-based management systems refer to the engagement and coordination of social and structural factors that focus on whole communities, states and entire nations, rather than individuals. Traditional health providers were not trained to work at this scale.
Public health professionals are trained to create healthy communities through prevention, education, and monitoring of community-wide chronic diseases in their patients. However, they too were unprepared to manage the increasing population-based decisions that the global pandemic demanded of them, yielding more political decision-making.
To handle this scale of challenges, public health professional’s major tool is current population data. At the global level, the WHO’s surveillance network collects data from all countries, but few national datasets can detect outbreaks or adequately warn relevant public health agencies and the public.
Many public health departments have previously struggled to successfully manage infectious disease outbreaks, such as the H1N1 and SARS epidemics. Past epidemics in the United States required added expertise and testing from the Centers for Disease Control and Prevention (CDC) to be sent to individual states, yet lessons learned for how to permanently provide more public health expertise to communities, states, and nations was not heeded.
Outcome: We must build a universal system for future global health challenges
Public health professionals normally work behind the scenes in prevention, preparedness, vaccines, and control of infectious and environmental diseases. They often describe themselves as being the “invisible health profession,” yet the people in the profession are largely responsible for the majority of improvements in global life expectancy.
It became increasingly clear that the key to success required public health professionals practicing population-based management with a strong public health multidisciplinary workforce, current population data, and leadership at all levels of society. For example, in the COVID-19 pandemic, this scale of management entailed identifying public safety measures—like social-distancing and mask-wearing to reduce the spread—as well as managing vaccine development and delivery and triaging the management of scarce resources. Many of these critical decisions were initially delayed, mismanaged, or ignored through political interference.
What must be done?
To improve global public health, the WHO should lead the creation of a global public health system. To support its adoption, the WHO must lead the creation of:
- a totally independent, highly resourced WHO and International Health Treaty with global authority under the United Nations;
- a highly trained, and multidisciplinary public health workforce focused on population-based management teams (PBMTs) that serve all population centers in every country;
- a global public health database that monitors, and keeps current the essential public health data that every PBMT requires, from the outset, to manage any outbreak, epidemic and pandemic worldwide;
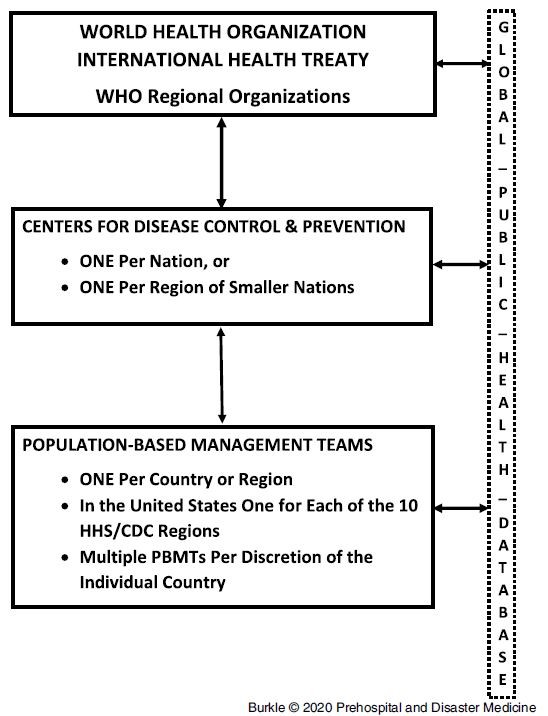
- and, the development of CDCs in every country or region (see Figure 1).
Under this model, permanent and highly trained PBMTs would be placed at each regional or country level CDC office and would be led by public health experts trained across the entire “disaster cycle” of crisis management (prevention, preparedness, response, rehabilitation, recovery). Figure 1 shows how the system would have PBMT professionals at national and international levels communicating and coordinating, along with the constant data provided by the global public health database. This would optimize the effectiveness at every level of the “disaster cycle” with emphasis on prevention and preparedness between pandemics and coordination of responses and recovery during and after the pandemics.
PBMTs would be managed by public health experts with interdisciplinary expertise, trained as Health Crisis Managers and Scientists. PBMTs would improve early detection, prevention, preparedness, and response in every community, basing their decisions on what the Global Public Health Database reveals on a daily basis. Similar to how traditional health providers are equipped with individual patient histories for those they serve, the global public health database would help the PBMTs understand, monitor, and respond rapidly to the region they serve.
In between crises, the regular updating and review of the global database would prepare the PBMTs to identify vulnerabilities that need attention, improve those vulnerabilities, and develop appropriate responses for when a future crisis hits. For instance, the social distancing and masking strategies developed for the current pandemic were developed through understanding population densities and pockets of vulnerable populations such as the poor and elderly.
CDCs in every country or region supported by the Global Public Health Database would report to both the WHO and relevant government authorities, building their role as an essential communications resource and nonpartisan decision-maker.
Conclusions: How to improve global health
We must demand a global public health system and create incentives to support it. This will involve addressing and managing more than just pandemics, as the Global Public Health Database could also alert and identify for public health decision-makers where lack of prevention and preparedness was contributing to worsening climate change, deforestation, unsustainable urbanization, population migrations, and work toward addressing multiple crises such as conflicts and food and water insecurity.
Non-medical professionals can also help improve the global public health system. Progress is being made. Over the last two decades, public health has gained considerable interest among the non-healthcare community, including students of the law and economics which will contribute greatly to the inter- and multidisciplinary demands and understanding of population-based public health decisions. Organizations such as the Wilson Center could use their unique expertise to develop a multidisciplinary forum for discussion and debate. Such organizations could help society identify where public health is lacking or potential avenues for mitigating these deficiencies in both policy and practice. Think tanks could also convene a forum for Deans of Schools of Public Health to debate how their responsibilities, roles, teachings, and multi-disciplinary decision-making roles for pending crises must be readdressed.
Public health must evolve from having a passive and narrow focus on health and medicine to taking the lead in the proposed global public health system. The model suggested here would institutionalize the global system and an increasingly interdisciplinary professional network would further support it.
Dr. Frederick M. Burkle, Jr., a retired professor, is now Senior Fellow and Scientist at the Harvard Humanitarian Initiative, Harvard University and Harvard T.H. Chan School of Public Health, and a Wilson Center Global Fellow.
Sources: Centers for Disease Control and Prevention, CNBC, Kaiser Family Foundation, Minnesota Department of Health Center for Public Health Nursing, Prehosp Disaster Med., The Harvard Gazette, and Tohoku J Exp Med.
Photo Credit: Massive rapid COVID-19 testing site, courtesy of faboi, Shutterstock.com.
 A Publication of the Stimson Center.
A Publication of the Stimson Center.