-
Population Age Structure: The Hidden Factor in COVID-19 Mortality
May 26, 2020 By Richard Cincotta
Until several months ago, demographers regarded a youthful age structure as an unequivocally detrimental demographic characteristic. Where more than half of the population is younger than age 25, countries are unable to attain high levels of economic and human capital development and face an increased risk of some forms of civil conflict. Yet, so far, during the ongoing pre-vaccine stage of the COVID-19 pandemic, the most age-structurally mature countries have been hardest hit by the disease. These countries are generally urbanized, wealthy, well-educated, and include a large proportion of seniors. And, somewhat surprisingly—despite being equipped with advanced medical technologies—these countries are experiencing the highest rates of mortality from complications related to COVID-19.
However, the epicenter of infection is shifting to populations in the remaining high-fertility, youthful regions of the world: into low-income countries in equatorial Africa and the Sahel, and into youthful clusters of states in the Middle East (Iraq, Syria, Gaza, and the West Bank) and South Asia (Afghanistan, Pakistan, Tajikistan, and the central-northern states of India). While these countries can expect COVID-19 to spread rapidly through the population, some analysts believe that the disease is unlikely to yield mortality rates (measured as deaths per million residents) rivaling those in either Europe or North America. With a lower level of age-structural vulnerability to COVID-19 mortality, limited capacity to treat or test, less ability to economically buffer populations in a lockdown, some analysts argue that governments in these regions may find that different strategies from those used in Europe and North America may save more lives.
In this brief note, I estimate the differences between the age-structural vulnerabilities to COVID-19 deaths of youthful countries and those of more mature populations in Europe and North America, and I discuss the demographic patterns in current data that highlight the importance of this factor.
Age-related Vulnerability
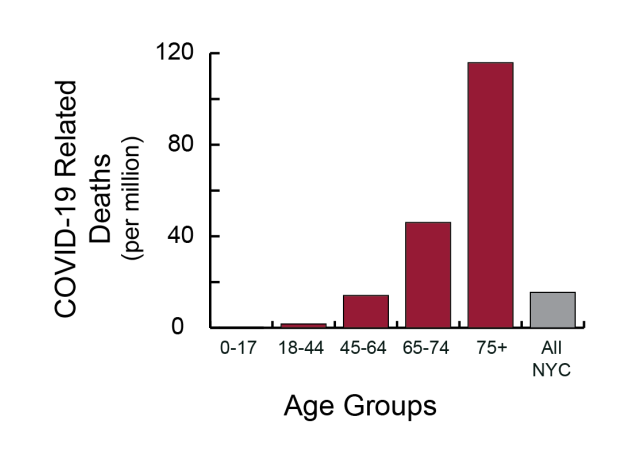
Estimates of COVID-19-related age-specific mortality rates in New York City have grown by leaps and bounds since reporting began two months ago. Today, at least 1 in 5 of the city’s residents have apparently been exposed to this coronavirus. Yet, the relationship between these rates has remained virtually constant (Fig. 1). By applying these age-related rates to individual countries, one can estimate the differences that might be observed, relative to a similar level of infection in New York City.

Differential Risks
As Figure 1 shows, seniors are most at risk. In New York City, deaths per million residents, ages 75 and older, has remained about 74 to 76 times the rate among 18- to 44-year olds over the past month. In addition, individuals with diabetes, or underlying respiratory, cardiac, or immune disorders are also at high risk, regardless of age. In contrast, those who are the least likely to die from COVID-19 complications are individuals in the youngest age groups, and they apparently are the least likely to exhibit symptoms.
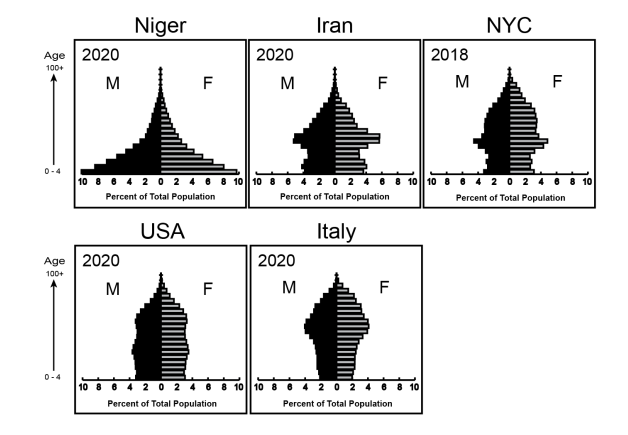
Differences in risks between countries in the Western Sahel and in Europe are nothing short of extraordinary. Note the differences in the pyramid-shaped age profile of Niger (in Fig. 2), and Italy’s muffin-shaped profile. For example, in Italy, residents ages 70 years and older (represented within the top one-third of the graph) currently make up 17 percent of the country’s population. In Niger, the world’s most youthful country, the situation is nearly opposite. The 70-plus group makes up just 1.5 percent of the population. In Niger, people under age 20 (represented by the bulging bottom one-fifth of the graph) comprise more than 60 percent of the population. In Italy, that same group makes up just 18 percent of its total population.

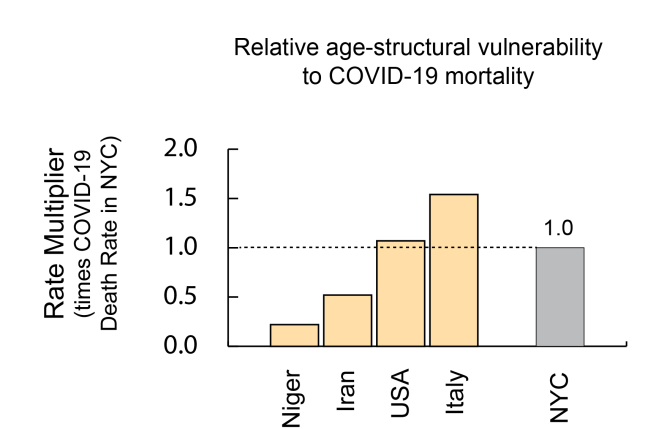
At present (May 20, 2020), New York City’s total COVID-19 mortality citywide rate is estimated at nearly 2,000 deaths per million residents. If Italy were to experience New York City’s age-specific COVID-19 mortality rates, Italy’s countrywide COVID-19 mortality (measured in deaths per million residents) would be expected to reach 1.5 times that of this city (Fig. 3). Fortunately, Italy’s countrywide mortality rate is far less. Applied to Niger, New York City’s age-specific rates would be expected to produce a countrywide mortality rate less than one-fifth of the city’s rate. According to this calculation, Italy’s age-structural vulnerability to COVID-19 mortality is about seven times greater than Niger’s.

Comparing Rates
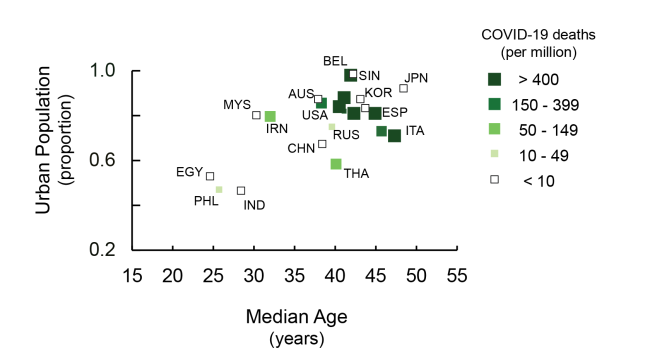
When graphed, the recent demographic pattern of COVID-19 mortality suggests a mixed picture. Age-structural vulnerability to COVID-19 mortality is apparent among the highly urbanized, age-structurally mature (high median age) countries of western and southern Europe (Fig. 4). These were late to respond to the pandemic and/or only weakly applied public health and social measures. While lagging Belgium (nearing 800 deaths per million), the United Kingdom, Spain, and Italy (each between 500 and 600 deaths per million), the COVID-19 mortality rate in the United States (currently nearing 300 deaths per million) may ultimately reach the 400 per million level and could significantly surpass it.
Where urbanized countries with mature populations have responded quickly to the COVID-19 pandemic or were prepared for an airborne viral outbreak, related countrywide mortality rates remain relatively low. Many countries in East and Southeast Asia have seen fewer than 10 deaths per million residents. Notably, early news commentaries that credited age structure as a factor in the COVID-19 mortality gap observed between South Korea and Italy are misplaced. While not as vulnerable as Italy’s population, South Korea has a mature age structure, but took earlier and more aggressive public health measures to contain the coronavirus than Italy. According to these calculations, South Korea’s age-structural vulnerability is about 70 percent of Italy’s. Yet, Italy’s countrywide COVID-19 mortality rate (per million residents) is more than 100 times the rate recorded in South Korea.

Reducing COVID-19 Mortality Below the Sahara
Although the age-structural vulnerability to COVID-19 mortality remains very low in the countries of equatorial Africa and the Sahel, the course of the pandemic in these countries is difficult to predict. Unfortunately, the public health conditions that are widespread in the most youthful, low-income countries—poor nutrition and sanitation, serious respiratory ailments (co-morbidities), cramped multi-generational living conditions, and low-capacity clinical facilities—could promote the disease’s spread and negate their age-structural advantage.
On the other hand, sub-Saharan African countries have some hidden strengths. Most African governments are focused on public health, rather than being pre-occupied with surgery and other expensive clinical procedures. For decades, their health ministries have built up their expertise and assembled protective equipment in order to combat other communicable diseases. Because of their particular strengths and vulnerabilities, some analysts advise that the low-income countries of sub-Saharan Africa should avoid “locking down” or implementing other restrictions that could severely deter important aspects of economic and social development, or cripple other ongoing public health efforts. Instead, they argue that these countries are likely to save the most lives by protecting the most vulnerable, and by encouraging the use of other WHO-recommended public health and social measures that reduce the spread of COVID-19.
Richard Cincotta is a Global Fellow at the Wilson Center’s Environment and Security Program. The author wishes to thank Barbara Crane for her comments and edits and the Population Institute for its support.
Sources: City of New York, Kaiser Family Foundation, LiveScience, UN Department of Economic and Social Affairs, World Bank, Center for Global Development.
Photo Credit: A crosswalk button in Minneapolis after the city disabled 450 walk buttons in late April 2020. Courtesy of Flickr user Chad Davis.
Topics: aging, Covid-19, demography, featured, global health, Guest Contributor, infectious diseases, population, youth
 A Publication of the Stimson Center.
A Publication of the Stimson Center.