-
CODE BLUE: Addressing NCDs in Maternal Health Starts with Increasing Access and Reducing Disparity
December 11, 2019 By Deekshita Ramanarayanan
We’ve got a crisis impacting our mothers and a crisis impacting our babies, said Dr. Lisa Waddell, Senior Vice President of Maternal Child Health and NICU Innovation and Impact Deputy Medical Director at the March of Dimes, at a recent Wilson Center event launching the Maternal Health Initiative’s CODE BLUE series, developed in partnership with EMD Serono, a business of Merck KGaA, Darmstadt, Germany. She was referring to non-communicable diseases (NCDs), which impact maternal health in the United States and globally. NCDs kill 18 million women of reproductive age each year, accounting for two in every three deaths among women.

We’ve got a crisis impacting our mothers and a crisis impacting our babies, said Dr. Lisa Waddell, Senior Vice President of Maternal Child Health and NICU Innovation and Impact Deputy Medical Director at the March of Dimes, at a recent Wilson Center event launching the Maternal Health Initiative’s CODE BLUE series, developed in partnership with EMD Serono, a business of Merck KGaA, Darmstadt, Germany. She was referring to non-communicable diseases (NCDs), which impact maternal health in the United States and globally. NCDs kill 18 million women of reproductive age each year, accounting for two in every three deaths among women.
Lack of Access: Maternity Care Deserts
In the United States, a lack of care poses a problem. Some 5 million women currently live in “maternity care deserts,” counties where no hospital offers obstetric services and where no maternal health providers work. “When you’re talking about the rise of diabetes and the rise of chronic health conditions—and then women are not able to get that care before pregnancy, can’t get that care during pregnancy—it should be no surprise that we’ve got these challenges,” said Dr. Waddell.
Barriers to accessing healthcare increase the risk of undiagnosed cardiovascular disease and other NCDs in pregnant women, said Dr. Wanda Nicholson, Director of the Diabetes and Obesity Core and Professor of Obstetrics and Gynecology at UNC-Chapel Hill and Immediate Past Fellow-at-Large with the American College of Obstetricians and Gynecologists (ACOG).
Inequity in access is also a global problem. For example, in target countries for the Ending Eclampsia project, women who lack of access to blood pressure monitors face increased risk of pre-eclampsia and postpartum hemorrhage, said Charlotte Warren, Director of the Ending Eclampsia Project and Maternal and Newborn Health Portfolio Lead at Population Council. Women in the project often had trouble getting the right information on how to prevent and treat NCDs. “They’re really not getting the care they should,” said Warren.
Disparities in Maternal Health
Lack of access to maternity care is often exacerbated by racial disparities in maternal health. In the United States, African American women are 3.3 times more likely to die from pregnancy and childbirth-related causes than white women. The prevalence of NCDs in the United States reflects these disparities. For example, African American women are three times more likely to die from cardiovascular disease than white women. And the maternal mortality rate for American Indian/Alaska Native women is 2.3 times higher than white women’s.
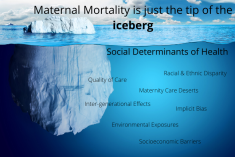
Maternal mortality is just the tip of the iceberg, said Dr. Waddell. Under the iceberg, underlying determinants like racism, systemic barriers in the health system, differences in economic stability, and different environmental exposures contribute to disparities in health outcomes. These determinants also contribute to gender disparities within the overall burden of NCDs. For example, in 2016, 1.5 million women died due to respiratory conditions, said Priya Kanayson, Policy and Advocacy Manager at NCD Alliance. Globally, women and girls are exposed to more indoor air pollution due to harmful cooking materials, which contributes to higher rates of respiratory disease. Poor treatment from a human relations standpoint can also lead to worse health. Disrespect and abuse during childbirth, for example, can contribute to negative birth outcomes and delay diagnosing symptoms of complications related to NCDs, said Warren.
Medical Mystery
Sometimes simply getting a correct diagnosis can be an uphill battle. For two years, Terrie Livingston, Head of Patient Outcomes & Solutions for Neurology and Immunology and Medical Affairs and Multiple Sclerosis Patient Advocate at EMD Serono, suffered from mysterious symptoms. After the birth of her second son, the symptoms intensified. “I had this profound fatigue that I didn’t have with my first child, where I couldn’t even move off the couch,” she said. “And it took every effort for me to be able to breastfeed my child.”
After experiencing short-term memory lapses, hearing problems, and vertigo, she went to see her doctor. Doctors first misdiagnosed her and treated her accordingly, but her symptoms persisted and worsened. Her whole right side became weak and it became hard to walk. Her doctors did not think that she had Multiple Sclerosis (MS), because she is not the typical MS patient, said Livingston, who is Asian American. MS was once thought to primarily affect white women, but African American women now have the highest rate of MS in the United States. In addition, the symptoms of MS are often common in otherwise healthy postpartum women, so providers often do not see them as a sign of something more, like MS.
Priorities Should Address Underlying Determinants
To tackle the maternal health crisis and address the impact of NCDs on maternal health, it is important to make maternity care more accessible to all people, said Dr. Waddell. Advocates in the United States have pushed to expand Medicaid insurance coverage for women from 60 days to one full year following pregnancy. Women who have a higher risk of developing cardiovascular conditions or other NCDs following pregnancy should be under continued surveillance and treatment past the first postpartum visit through one full year after childbirth, said Dr. Nicholson. And collaboration in maternal health should go beyond the “OB/GYN world” and include midwives and nurse practitioners, she said, especially in rural areas and “maternity care deserts.”
In order to address social norms and racial disparities in health outcomes, we need to start with the social determinants of health, said Dr. Nicholson. Health systems should also prioritize implicit bias and cultural competency training for providers to reduce the barriers that minority women face in the healthcare system and improve health outcomes. Globally, more work needs to be done to improve women’s experiences in healthcare settings, said Warren.
Taking a Life-Course Perspective
Non-communicable diseases can have an “intergenerational effect,” said Kanayson. Children of women with NCDs face a higher risk of developing NCDs throughout their own lifespans. In order to fully address the impact of NCDs on maternal health, we need to make an effort to look further upstream to focus on interventions to reduce NCD risk factors even prior to conception, said Dr. Nicholson. A prevention-based model rather than a treatment-based model would address NCDs before they cause complications in pregnancy or later in life, the panelists said.
Women should be the center of care, said Warren. “They should be treated as individuals. And it doesn’t matter who they are, what they are, or where they come from, but we really need to focus on the woman and her lifestyle, and how to help her have a healthy life.”
Sources: Centers for Disease Prevention and Control, The Kirwan Institute for the Study of Race and Ethnicity, U.S. Department of Health and Human Services Office of Population Affairs, White Ribbon Alliance.
Photo Credit: Photo via Shutterstock. All rights reserved.
 A Publication of the Stimson Center.
A Publication of the Stimson Center.