-
Combining Health and Food Security in Mozambique: Interview With Pathfinder International’s SCIP Project
May 15, 2013 By Carolyn Lamere
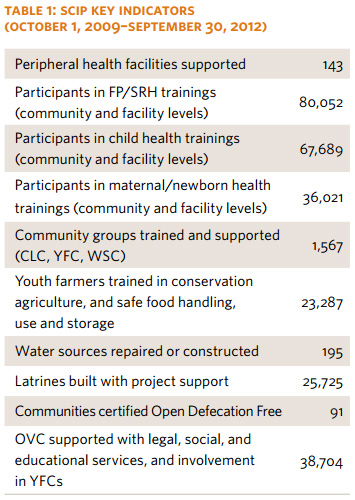
Pathfinder International’s Strengthening Communities Through Integrated Programming (SCIP) is part of a new push towards integrated development – looking at communities as a whole and addressing multiple, traditionally-siloed sectors at once. SCIP integrates both its activities and its funding to great effect in Mozambique.
SCIP was slated to discuss their experience at the Wilson Center in March, but the event was canceled due to inclement weather. We did, however, manage to get this interview up. Enjoy!
What is SCIP and who are your partners?
SCIP is a five-year project begun in 2009 in Nampula province, Mozambique, designed to improve quality of life at the household and community level by improving health and nutrition status and increasing household economic viability. Funded by the U.S. Agency for International Development (USAID), the project combines health goals – including family planning, reproductive health, water, and sanitation – and conservation farming.
SCIP is led by Pathfinder International but incorporates efforts by Population Services International, World Relief, CARE International, Cooperative League of the United States of America, and the Mozambican government. The Governor of Nampula province has welcomed the SCIP team with enthusiasm, highlighting the tremendous potential of the project to improve health conditions in communities across the 14 focus districts. He committed to facilitating implementation by “opening the doors” with key administrators and directed SCIP to work with the Unit of Coordination for Nampula Development, which coordinates between civil society partners in the province.
What characteristics distinguish Nampula from the rest of Mozambique? Why combine health and conservation goals?
Nampula province is the most densely populated area of Mozambique. It has favorable agro-ecological conditions, with better agricultural potential than much of the country, yet poverty and poor health are pervasive.
Demographic and Health Survey data from 2003 found an infant mortality rate of 101 per 1,000 live births in Nampula, the second highest in the country. Nearly half of children under age five were found to be stunted; only 51 percent of children under one completed immunization; and female literacy was just 20 percent.
More recent surveys have found that contraceptive prevalence is very low (3.8 percent, according to a 2008 Multi-Indicator Cluster Survey), less than half the population has access to safe drinking water (43.1 percent), and HIV prevalence among people 15 to 49 years is 4.6 percent.
Land degradation, deforestation, and erosion are also major concerns for farming and food security.
Integration across health sectors, like family planning and HIV/AIDS, and between health and non-health programs, like water, sanitation, hygiene, and farming, amplifies the impact of SCIP’s programs.
How did you decide to work on integrated programming instead of taking a more traditional route?
We know that funding is generally targeted to specific technical areas: health, economic growth, environment activities, etc. Even within health funding, we have divisions between HIV prevention, treatment, and community support; maternal and child health; and family planning. In reality we know these are all best dealt with in an integrated fashion.
As such, when the original request for proposal from USAID called for both integrated activities and funding streams, we saw this as a real opportunity to bring partners together into one common organization in a coordinated manner. All the SCIP partners work in the same offices in Nampula and at district levels, sharing logistics and a common monitoring and evaluation system, which greatly facilitates communication, collaboration, and efficient use of resources.
Integration brings together common functions within and between organizations to solve common problems and develops a commitment to shared vision and goals.
SCIP’s approach to integration represents a benchmark in Mozambique, as it is deeply aligned with the National Health System’s current policy of decentralization alongside more community involvement. Integration and decentralization ensure higher chances for universal access and more control over health production.
Can you explain the role of “community leader councils”?
 SCIP directs a substantial amount of effort to community-based programming. Our community-based interventions are based on close collaboration with what we call “community leader councils” (CLCs) – small units made up of existing leaders (civil, traditional, and religious), which can serve as an entry point into a community and create a favorable environment for increasing the availability of services. CLCs are really the cornerstone of integration for SCIP. They are often ideally placed to facilitate coordination across stakeholders and technical areas, and help prompt community-driven action to solve health and development problems.
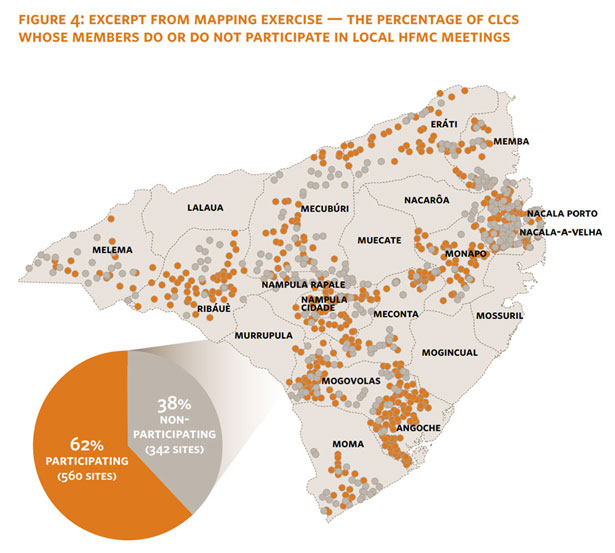
SCIP directs a substantial amount of effort to community-based programming. Our community-based interventions are based on close collaboration with what we call “community leader councils” (CLCs) – small units made up of existing leaders (civil, traditional, and religious), which can serve as an entry point into a community and create a favorable environment for increasing the availability of services. CLCs are really the cornerstone of integration for SCIP. They are often ideally placed to facilitate coordination across stakeholders and technical areas, and help prompt community-driven action to solve health and development problems.As such, SCIP organizes meetings with CLCs to discuss community involvement in the 14 districts. The rate at which these CLCs review data and support community health workers is an approximation of their accountability to the people they serve, and based on a mapping exercise undertaken in August 2012, 87 percent of the 906 CLCs in the 14 districts we work in were meeting regularly.
Has the project made greater progress in one sector or another? If so, why?
The project has seen significant progress in many areas, not just one in particular. But there are particularly promising results in improving access to family planning and increasing community involvement.
Family planning services available to the districts we work in, measured in couple-years of protection (CYP – the estimated protection provided by family planning services during a one-year period, based upon the volume of all contraceptives sold or distributed free of charge to clients during that period), have increased from enough to cover just 4 percent of women of reproductive age at the end of year one to 10 percent at the end of year three.
 This is rewarding to see, given the number of program activities that take place promoting family planning through all the project’s components. For example, health providers are encouraged to talk about family planning with their clients through on-the-job training and regular supportive supervision. They also are trained in meetings to discuss family planning and related issues through “Hot Topics” – a dynamic approach the SCIP team developed to encourage community dialogue and exchange around norm shifting and behavior change. Family planning is also covered by community health workers in their home visits, and many of these same workers facilitate sessions on family planning with youth farmer clubs. Community-based HIV testers/counselors also include discussions about family planning during their sessions with clients.
This is rewarding to see, given the number of program activities that take place promoting family planning through all the project’s components. For example, health providers are encouraged to talk about family planning with their clients through on-the-job training and regular supportive supervision. They also are trained in meetings to discuss family planning and related issues through “Hot Topics” – a dynamic approach the SCIP team developed to encourage community dialogue and exchange around norm shifting and behavior change. Family planning is also covered by community health workers in their home visits, and many of these same workers facilitate sessions on family planning with youth farmer clubs. Community-based HIV testers/counselors also include discussions about family planning during their sessions with clients.We’ve also increased the coverage of new users of family planning services at health facilities.
SCIP has done a lot of work to strengthen the link between the existing public health system and communities, working from both sides to reinforce the zone of interaction between the two.
We’ve also established effective partnerships with local government for building and maintaining water sources, rehabilitating peripheral health facilities, building maternal waiting homes, and revitalizing platforms for improved service delivery, transparency, and good governance.
Has the project struggled with any particular area?
One challenge is that we are doing all of this interesting work but it has been difficult to document. This is for a variety of reasons: the complexity of the project, the types of data readily available (or not, given the data quality issues inherent in many countries’ national service statistics), and variation between districts.
In order to address this, we are intensifying our efforts for improved data collection with partners, looking at best practices in the field, and studying specific activities in depth rather than trying to document everything. We hope to feed what we learn back into our implementation plan and disseminate it with broader audiences.
We are also creating “integration indicators” that measure progress around integrated approaches. Some examples of integration indicators are: the proportion of youth farmers’ clubs members who are counseled and tested for HIV; the proportion of HIV positive clients who received a family planning method or referral after counseling; and the number of households with chronically ill patients and a toilet.
Documentation has been a challenge but something that we value and are prioritizing as we enter our fourth year of implementation.
What is the future of SCIP in Nampula? Do you see the changes you’ve helped bring about as sustainable?
Sustainability of the changes brought about by SCIP rely extensively on existing systems and structures and building the capacity of health workers, health activists, and community leaders .
To that end, SCIP will continue to build capacity of community structures and networks, increasing their engagement with the formal health system to improve accountability, demand for, and access to quality health services. With provincial support, and district- and community-level commitment, the SCIP consortium will maintain its role as a mechanism for implementation of government health strategies, while catalyzing transformational change at the community level.
Image Credit: “Empowering Communities Through Integrated Systems Strengthening in Northern Mozambique,” courtesy of Alicia Mehl/SCIP. Map and Chart: SCIP.
 A Publication of the Stimson Center.
A Publication of the Stimson Center.